Cure for Blepharitis?
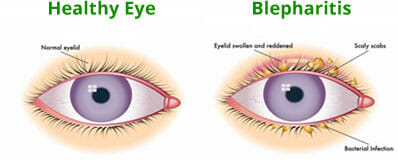
People who suffer from Blepharitis – inflammation of the eye lids — are looking for a cure.
The question is – “Is There a cure?”
Blepharitis and dry eyes often concur – they are linked. Many people who suffer from it find that this common eye condition can recur and make dry eyes even worse. It can affect both men and women, children and adults, and is not limited to any particular ethnicity. Therefore, treatment for this condition is commonly needed. If you have this condition and dry eyes, the simple answer is – “There is no cure”
TheraLife carries a complete line of all-natural relief products for both conditions.
We can help you manage this condition, prevent vision damage and make your life a whole lot easier.
Blepharitis Facts
Blepharitis is a condition that affects the base of the eyelashes. It can be present in front or behind the eyelid. Classified as either chronic or acute, adults are the most common suffers.
When the condition is acute, blepharitis is often referred to as an eyelid infection. However, when inflammation is chronic, blepharitis is often the diagnosis. Blepharitis is thought to affect almost half of patients who visit an eye doctor.
When this condition is located on the front of the upper eyelid, it is referred to as anterior blepharitis and is similar to dandruff on the scalp. If located on the inside of the upper eyelids, it is called posterior blepharitis.
Since the glands that secrete lubricating oil to thicken tears are located on upper and lower eye lids, dry eyes often accompany posterior blepharitis.
Symptoms
The signs of blepharitis can be seen on the eyelids and include:
- Redness of the eyes or eyelids
- Itchiness on or around the eyes
- Flacking skin on the edge of the eyelids
- Crusting at the base of the lashes that may be more prominent in the morning
- A feeling of burning, itching, or grittiness on the eyes
- Excessive tear production
- Sticky eyes
- Sensitivity to light
- Inability to wear contact lenses
Although not a sight-threatening problem, it can decrease a person’s vision. Therefore, treatment is vital to improve quality of life.
Diagnosis
An eye doctor will determine if a patient has anterior or posterior blepharitis. Using a slit lamp is helpful in revealing looking for crusty sticky build up on the eye lashes with bacteria or mites attached to the lashes.
Anterior blepharitis is often diagnosed when the following symptoms are present:
- Redness and swelling of the eyelid
- Increased size of the blood vessels on the outside of the eyelid
- Flaky skin on the base of the outer part of the eyelash base
- In severe cases, eyelashes that point inward, toward the eye
- Loss of color of the eyelashes
- Loss of eyelashes
- Scarring of the eyelid or cornea
Posterior blepharitis is often diagnosed when the following symptoms are present:
- Glands located at the base of the eyelashes that are blocked or dilated
- Thick secretion of oil from the glands
- Scaring on the lid around the glands
Eyelids that are red and sticky with clumps of scaly skin located around the base of the eyelashes can be soothed with a hot compress applied twice a day to the affected area.
Once the crusty skin is loosened, gentle cleaning of the area can remove this dead skin. TheraLife offers a complete line of natural eye care products that can relieve the symptoms of blepharitis.
The best eye lid cleanser is hypochlor based where it works by disrupting the biofilm layer where bacteria or mites to anchor, therefore preventing re-attachment.
Detergent based eye lid cleanser tend to clean off the debri, but also strips off precious lubricantion secreted by the meibomian glands.
Treatment
As a leader in chronic dry eye relief, TheraLife goes directly to the source of blepharitis, naturally treating underactive tear secretion, the root cause of both conditions.
Targeting this issue from the inside out, TheraLife provides the body with the natural ability to produce tears which can eliminate painful, irritated, and dry eyes. Now with the ability to eliminate the need for constant eye drops,
TheraLife users are finding that their eye pain, redness, and dryness disappear naturally with use of their complete line of blepharitis solutions.
Once dry eye is under control by eliminating inflammation, blepharitis will also be under control with proper lid hygiene.
- HypoChlor Cleanser – Containing hypochlor, this natural cleanser prevents reattachment of mites and bacteria to the biofilm layer of the eye lid.
- TheraLife Eye Capsules – Helping to restore the natural tear secretion to eyes, the clinically-proven ingredients in these natural capsules help stop the dry eye cycle and bring a healthier, long-term solution to dry eye treatment
- Fish Oil – A natural tear thickening and inflammation fighting agent
- Hot Compress – Stays hot for a prolonged period of time allowing the meibomian glands to unclog and function normally.
TheraLife All-In-One Starter Kit includes: Best Treatment For Recovvery
- 4 bottles of TheraLife Eye
- 1 bottle of molecularly distilled purified Fish Oil
- 1 bottle of eye lid cleanser
- 1 gel hot compress
- 90-day money back guarantee
There is no cure for Blepahritis and dry eyes, but there is help that can make your life normal again.
Don’t suffer another day with painful, red, and irritated dry eyes. Let TheraLife help bring natural relief to dry eyes.
Frequently Asked Questions
How do you get rid of blepharitis fast?
The fastest way is to use antibiotic oitments, use warm compresses, cleaning eyelids afterwards,. Remember to treat dry eyes since it is the root cause of blepharitis to begin with.
What is the best ointment for blepharitis?
The best ointment for blepharitis is antibiotics. This is because most blepharitis is caused by bacteria, especially staphylococcus.
How long does blepharitis take to clear up?
If this is your first time contracting blepharitis, it should take about 2 weeks to clear up. However, if you don’t treat your dry eyes, the blepharitis can become chronic and very difficult to get rid of. Be sure to treat your dry eyes at the same time with TheraLife.
How do you get rid of blepharitis on your eyelid?
Blepharitis on your eyelid is crusty, sticky and difficult to clean. The best way is to use a wet warm compress, place on your eyelids for 10 minutes , gently massage the eyelid followed by cleaning the eyelids with an eyelid cleanser like Avenova. Be sure to treat your dry eyes with TheraLife to avoid blepharitis becoming chronic.
How do I know if I’ve got blepharitis?
You will know when you have blepharitis because you are waking up every morning with your eyelids stuck together. The crusty and sticky buildup on your eyelids can be very uncomfortable. Your eyelids are swollen, red and flaky. It is time for you to visit your eye doctor to begin proper treatment.
Conclusion
In conclusion, dry eye is a multifactorial disease of the tears and the ocular surface, a system formed by several structures working together to protect the eye from excessive environmental and biological stress. Treating dry eye is critical in blepharitis recovery. Left untreated can lead to cornea damage. Seek help from your eye doctor to determine the best treatment options.
References
Barabino S, Montaldo E, Solignani F, Valente C, Mingari MC, Rolando M. Immune response in the conjunctival epithelium of patients with dry eye. Exp Eye Res. (2010) 91:524–9. doi: 10.1016/j.exer.2010.07.008
32. McClellan AJ, Volpe EA, Zhang X, Darlington GJ, Li DQ, Pflugfelder SC, et al. Ocular surface disease and dacryoadenitis in aging C57BL/6 mice. Am J Pathol. (2014) 184:631–43. doi: 10.1016/j.ajpath.2013.11.019
33. Subbarayal B, Chauhan SK, Di Zazzo A, Dana R. IL-17 augments B cell activation in ocular surface autoimmunity. J Immunol. (2016) 197:3464–70. doi: 10.4049/jimmunol.1502641
34. Tsubota K, Pflugfelder SC, Liu Z, Baudouin C, Kim HM, Messmer EM, et al. Defining dry eye from a clinical perspective. Int J Mol Sci. (2020) 21:9271. doi: 10.3390/ijms21239271
35. Yu L, Yu C, Dong H, Mu Y, Zhang R, Zhang Q, et al. Recent Developments About the Pathogenesis of Dry Eye Disease: Based on Immune Inflammatory Mechanisms. Front Pharmacol. (2021) 12:732887. doi: 10.3389/fphar.2021.732887
36. Sekhon AS, He B, Iovieno A, Yeung SN. Pathophysiology of corneal endothelial cell loss in dry eye disease and other inflammatory ocular disorders. Ocul Immunol Inflamm. (2021) 1–11. doi: 10.1080/09273948.2021.1980808
37. Ponzini E, Scotti L, Grandori R, Tavazzi S, Zambon A. Lactoferrin concentration in human tears and ocular diseases: a meta-analysis. Invest Ophthalmol Vis Sci. (2020) 61:9. doi: 10.1167/iovs.61.12.9
38. Zhang Y, Lu C, Zhang J. Lactoferrin and its detection methods: a review. Nutrients. (2021) 13:2492. doi: 10.3390/nu13082492
39. van Setten GB. Osmokinetics: A new dynamic concept in dry eye disease. J Fr Ophtalmol. (2019) 42:221–5. doi: 10.1016/j.jfo.2018.11.001
40. Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci. (2006) 47:4309–15. doi: 10.1167/iovs.05-1504
41. Suzuki M, Massingale ML, Ye F, Godbold J, Elfassy T, Vallabhajosyula M, et al. Tear osmolarity as a biomarker for dry eye disease severity. Invest Ophthalmol Vis Sci. (2010) 51:4557–61. doi: 10.1167/iovs.09-4596
42. VanDerMeid KR, Su SP, Ward KW, Zhang JZ. Correlation of tear inflammatory cytokines and matrix metalloproteinases with four dry eye diagnostic tests. Invest Ophthalmol Vis Sci. (2012) 53:1512–8. doi: 10.1167/iovs.11-7627
43. Luo L, Li DQ, Doshi A, Farley W, Corrales RM, Pflugfelder SC. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Invest Ophthalmol Vis Sci. (2004) 45:4293–301. doi: 10.1167/iovs.03-1145
44. Li DQ, Luo L, Chen Z, Kim HS, Song XJ, Pflugfelder SC, et al. and ERK MAP kinases mediate induction of IL-1beta, TNF-alpha and IL-8 following hyperosmolar stress in human limbal epithelial cells. Exp Eye Res. (2006) 82:588–96. doi: 10.1016/j.exer.2005.08.019
45. Shimizu T, Nakamura H, Kawakami A. Role of the innate immunity signaling pathway in the pathogenesis of sjogren’s syndrome. Int J Mol Sci. (2021) 22:3090. doi: 10.3390/ijms22063090
46. Simmons KT, Xiao Y, Pflugfelder SC, de Paiva CS. Inflammatory response to lipopolysaccharide on the ocular surface in a murine dry eye model. Invest Ophthalmol Vis Sci. (2016) 57:2443–51. doi: 10.1167/iovs.15-18396
47. Karin N. CXCR3 ligands in cancer and autoimmunity, chemoattraction of effector t cells, and beyond. Front Immunol. (2020) 11:976. doi: 10.3389/fimmu.2020.00976
48. Perez VL, Stern ME, Pflugfelder SC. Inflammatory basis for dry eye disease flares. Exp Eye Res. (2020) 201:108294. doi: 10.1016/j.exer.2020.108294
49. Haber SL, Benson V, Buckway CJ, Gonzales JM, Romanet D, Scholes B. Lifitegrast: a novel drug for patients with dry eye disease. Ther Adv Ophthalmol. (2019) 11:2515841419870366. doi: 10.1177/2515841419870366
50. An S, Raju I, Surenkhuu B, Kwon JE, Gulati S, Karaman M, et al. Neutrophil extracellular traps (NETs) contribute to pathological changes of ocular graft-vs-host disease (oGVHD) dry eye: Implications for novel biomarkers and therapeutic strategies. Ocul Surf. (2019) 17:589–614. doi: 10.1016/j.jtos.2019.03.010
51. Galletti JG, de Paiva CS. The ocular surface immune system through the eyes of aging. Ocul Surf. (2021) 20:139–62. doi: 10.1016/j.jtos.2021.02.007
52. Ho TC, Yeh SI, Chen SL, Tsao YP. Integrin alphav and vitronectin prime macrophage-related inflammation and contribute the development of dry eye disease. Int J Mol Sci. (2021) 22:8410. doi: 10.3390/ijms22168410
53. Steven P, Schwab S, Kiesewetter A, Saban DR, Stern ME, Gehlsen U. Disease-specific expression of conjunctiva associated lymphoid tissue (CALT) in mouse models of dry eye disease and ocular allergy. Int J Mol Sci. (2020) 21:7514. doi: 10.3390/ijms21207514
54. Willcox MDP, Argueso P, Georgiev GA, Holopainen JM, Laurie GW, Millar TJ, et al. TFOS DEWS II tear film report. Ocul Surf. (2017) 15:366–403. doi: 10.1016/j.jtos.2017.03.006
55. Pflugfelder SC, Corrales RM, de Paiva CS. T helper cytokines in dry eye disease. Exp Eye Res. (2013) 117:118–25. doi: 10.1016/j.exer.2013.08.013





I have ocular rosacea and blepharitis – is the treatment any different in this case. My right eye is very sore and I cannot cope with bright sunlight. I am fearful my eyesight will be affected. I use a heated pad and eyelid wipes as a current ongoing treatment,
This information was developed by the National Eye Institute to help patients and their families search for general information about blepharitis. An eye care professional who has examined the patient’s eyes and is familiar with his or her medical history is the best person to answer specific questions.
Nice comment. Call if you have any questions. 1-877-917-1989
Thanks for sharing such wonderful knowledge! Natural Treatment for Blepharitis that can be used to treats and gets rid of blepharitis.
There is a cure for blepharitis. Both dry eyes and blepharitis must be treated at the same time. There is no cure for dry eyes however. TheraLife Eye capsule is ideal in treating dry eyes long term. It is natural, effective and help you produce your own tears for dry eye relief. Learn more from TheraLIfe . Call toll free from United States and Canada 1-877-917-1989