Iritis Treatment Naturally

- Powerful Iritis Relief From Inside Out
- Strong Anti-inflammatories Directly To your Eyes
- Restore & Revive Your Own Tear Functions
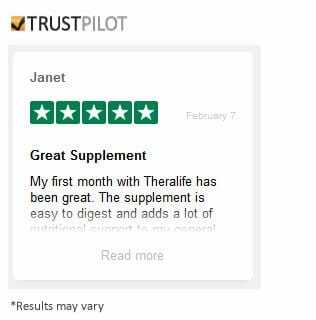
Testimonials
“I must say I see a tremendous improvement after one month; the inflammation is down. My dry eye and Iritis symptoms are also gone. So glad I found TheraLife.”
–Gini- North Carolina, USA
*Results may vary
Call and talk to a doctor if TheraLife is right for you- 1-877-917-1989 US/Canada
Iritis Home Treatment Naturally
What is Iritis?
Iritis is the inflammation of the color part of your eye. It is also called “Anterior Uveitis.”
What are the symptoms of Iritis?
Symptoms of Iritis can happen all of a sudden and develop rapidly over a few hours or days.
What is acute Iritis
Acute Iritis causes eye pain, blurred vision, headache, light sensitivity, red eyes, and vision loss. Steroid eye drops are great for immediate intervention. With quick intervention, the outcome expected to be good.
Conventional treatment for Iritis-steroid drops
The conventional treatment for Iritis from your eye doctor will include steroid drops to control inflammation for Iritis (anterior uveitis). But Steroids cause an increase in eye pressure (Glaucoma). For some, steroids are not an option. Iritis left untreated can cause permanent vision loss.
TheraLife’s Natural Treatments for Iritis
TheraLife Eye is a powerful natural alternative to steroids to fight Iritis -eye inflammation. Taking Theralife Eye capsules can help you prevent Iritis recurrence without the use of steroid eye drops.
The TheraLife Discount Bundle
TheraLife Eye Enhanced (One Month) Bundle, which includes 4 bottles of TheraLife Eye Enhanced and 1 bottle of Omega-3 Fish Oil. The one month bundle typically retails for $150, but you can get it on sale now for the discount price of $140. 
Why is Acute Iritis Treatment Immediately Important?
Sudden onset of Iritis with eye pain, blurred vision, light sensitivity can be very frightening. Go to your eye doctor and get Iritis treatment right away. Untreated Iritis could lead to vision loss and even blindness. Immediate treatment for Iritis often has excellent outcomes. So don’t delay. In general, Iritis is not contagious
Iritis and Dry Eyes
Inflammation of the eye, such as from Dry Eyes and Blepharitis, can cause Iritis. It is common for people who recover from Iritis to have dry eyes. They start complaining about blurred vision, foreign body sensation, light sensitivity, and yet Iritis is no longer an issue.
Autoimmune diseases can cause Iritis
Other pre-existing conditions such as infections, autoimmune diseases can also cause Iritis. Find out if you have any of the risk factors for chronic dry eyes, click here.
Challenges with Conventional Iritis Treatment
The first line of defense for Iritis is steroid eye drops to reduce eye inflammation; and or dilating eye drops, which can reduce the pain of the iris. Unfortunately, steroid drops can cause high intraocular pressure (IOP), resulting in Glaucoma, which can cause blindness.
Why TheraLife For Iritis?
TheraLife Eye capsule is an all-natural formula that reduce inflammation and delivers to the eye without the steroid side effects. TheraLife has treatment options for both Iritis, Dry Eyes, and Autoimmune Diseases. TheraLife Eye capsules are clinically proven to relieve dry eyes from inside out, without eye drops. Clinical results show TheraLife Eye to be effective and safe when eye drops don’t work. . To learn more, click here. TheraLife has a patented formula for Autoimmune dry eyes, in case the cause of your Iritis is autoimmune related. Learn more
Do Acute Iritis Recur and Come Back?
Once you have Iritis, it will come back at a later time. Iritis recurrence is particularly true if you have underlying inflammatory diseases. Some people get it only once, especially if they take precautions to prevent it from recurring.
What Causes Iritis?
- Trauma – In most cases, stress or trauma causes Iritis. Examples are burns, punctures, or strikes with a blunt object. This is called traumatic iritis.
- Chronic Dry Eyes, Blepharitis – inflammation of the eyes.
- Autoimmune Diseases. People who are susceptible to Acute Iritis are those with autoimmune diseases. Examples are Ankylosing spondylitis ( a type of arthritis), Reactive Arthritis, Inflammatory Bowel Disease, Bechet’s Disease, and Psoriatic Arthritis are known to cause Iritis. Gene alteration in autoimmune diseases makes white blood cells attack one’s tissues, causing Iritis.
- Inflammatory Infections can causes Iritis.Iritis can be related to diseases or infections, such as arthritis, tuberculosis, syphilis, tonsils, sinus, kidney, gallbladder, and teeth.
What are the Symptoms of Iritis?
These symptoms can affect either one eye or both eyes. Common complaints are:
- Eye pain
- VisionLoss
- Red-eye
- Lightsensitivity
- Headache
- Reducedvision,
- Misshapedpupils
Diagnosis of Iritis
Your eye doctor can look into a slit lamp microscope and assess for the possible cause of Iritis. And if you have an infection. Your eye doctor may also order additional tests to rule out other possibilities.
- Tests for autoimmune diseases
- Tests for infections, either viral or bacterial.
- Chest X-Ray or CT scans of the chest to rule out tuberculosis, sarcoidosis.
When to Start Iritis Treatment
It depends on how severe the Iritis is. Treatment starts as soon as possible to prevent the condition from getting any worse. The symptom progression can be very rapid. Typical approaches include:
- Antibiotics to treat bacterial eye infection
- Anti-viral medications to treat viral infections. E.g., Herpes
- Steroid eye drops, or oral steroids to reduce inflammation
- Eye drops to dilate your pupils to minimize pain and prevent complications.
- Autoimmune diseases, immune-suppressive medications may be used.
These treatments can be delivered in the form of eye drops, orally, or through an IV (intravenous). Or as a shot around or into your eye.
Complications of Iritis
Most often, Immediate treatment of Iritis does not cause other complications. However, possibilities do exist for:
- Glaucoma – caused by steroid use.
- Cataract – Caused by steroid use
- Inflammation of the vitreous fluid inside your eyeball
- Inflammation of the retina
- Optic nerve damage – in severe cases causing blindness
- Macular Edema – swelling of the central part of the retina.
- Calcium deposits on your cornea, causing damage.
Can Iritis be prevented?
Treat your dry eyes, autoimmune diseases to decrease your chances of getting Iritis. TheraLife has multiple treatment options for you. Chronic dry eye, Blepharitis, and MGD – Relieve symptoms and get rid of Blepharitis, recovery from MGD. All-natural treatments from inside out. Chronic Dry Eye Starter KitAutoimmuneDry Eye Control – TheraLife Eye Autoimmune formula designed explicitly to relieve dry eyes, reduce inflammation, and autoimmune flares. To learn more – click here
References
1.Watad A, Bridgewood C, Russell T, Marzo-Ortega H, Cuthbert R, McGonagle D. The Early Phases of Ankylosing Spondylitis: Emerging Insights From Clinical and Basic Science. Front Immunol. 2018;9:2668.
2.Kaufman AR, Myers EM, Moster ML, Stanley J, Kline LB, Golnik KC. Herpes Zoster Optic Neuropathy. J Neuroophthalmol. 2018 Jun;38(2):179-189.
3.Krishna U, Ajanaku D, Denniston AK, Gkika T. Uveitis: a sight-threatening disease which can impact all systems. Postgrad Med J. 2017 Dec;93(1106):766-773.
4.Okuma H, Hashimoto K, Wang X, Ohkiba N, Murooka N, Akizuki N, Inazawa T, Ogawa Y. Systemic Sarcoidosis with Thyroid Involvement. Intern Med. 2017 Aug 15;56(16):2181-2186.
5.Reddy AK, Engelhard SB, Shah CT, Sim AJ, Thorne JE. Medical Malpractice in Uveitis: A Review of Clinical Entities and Outcomes. Ocul Immunol Inflamm. 2018;26(2):242-248.
6.Harthan JS, Opitz DL, Fromstein SR, Morettin CE. Diagnosis and treatment of anterior uveitis: optometric management. Clin Optom (Auckl). 2016;8:23-35.
7.Delwig A, Keenan JD, Margolis TP. Topical Valganciclovir for the Treatment of Hypertensive Anterior Uveitis. Cornea. 2015 Nov;34(11):1513-5.
8.Alkhayyal MA, Stone DU. Practice patterns for herpes simplex keratitis: A survey of ophthalmologists in Gulf Coast countries. Saudi J Ophthalmol. 2017 Apr-Jun;31(2):61-64.
9.Lee MI, Lee AW, Sumsion SM, Gorchynski JA. Don’t Forget What You Can’t See: A Case of Ocular Syphilis. West J Emerg Med. 2016 Jul;17(4):473-6.
10.Kujundzić M. [The role of biologic therapy in the treatment of extraintestinal manifestations and complications of inflammatory bowel disease]. Acta Med Croatica. 2013 Apr;67(2):195-201. [PubMed]
11.Adio AO, Alikor A, Awoyesuku E. Survey of pediatric ophthalmic diagnoses in a teaching hospital in Nigeria. Niger J Med. 2011 Jan-Mar;20(1):105-8.
12.Engelhard SB, Patrie J, Prenshaw J, Bajwa A, Monahan R, Reddy AK. Traumatic uveitis in the mid-Atlantic United States. Clin Ophthalmol. 2015;9:1869-74.
13.Snell RS, Lemp MA. The eyeball. In: Snell RS, Lemp MA, editors. Clinical Anatomy of the Eye. 2nd ed. Malden, MA: Blackwell Science; 1998:140–156.
14.Rao NA, Forster DJ. Basic principles. In: Podos SM, Yanoff M, editors. The Uvea, Uveitis, and Intraocular Neoplasms. Vol 2. New York: Gower Medical Publications; 1992:1–17.
15.Huang JJ, Gau PA. Ocular Inflammatory Disease and Uveitis Manual. Diagnosis and Treatment. Philadelphia: Lippincott Williams & Wilkins; 2010:1–9.
16.Foster CS, Vitale AT. Diagnosis and Treatment of Uveitis. 2nd ed. New Delhi: Jaypee Brothers Medical Publishers Ltd; 2013:20–32.
17.Smit RLMJ, Baarsman GS, DeVries J. Classification of 750 consecutive uveitis patients in the Rotterdam Eye Hospital. Int Ophthalmol. 1993;17:71–75.
18.Silverstein A. Changing trends in the etiological diagnosis of uveitis. Documenta Ophthalmologic. 1997;94:25–37.
19.Roday MJH, Stilma JS, Rothova A. Blindness from uveitis in a hospital population in Sierra Leone. Br J Ophthalmol. 1994;9:690–693.
20.Rothova A, Suttorp-van Schulten MSA, Treffers WF, et al. Causes and frequency of blindness in patients with intraocular inflammatory diseases. Br J Ophthalmol. 1992;70:137–141.
21.Whitley W, Sheppard J. The basics of uveitis. Rev Optom. 2011.
22.Smith RE, Nozik RM. Uveitis: A Clinical Approach to Diagnosis and Management. Baltimore: Williams & Wilkins; 1983.
23.Gutteridge IF, Hall AJ. Acute anterior uveitis in primary care. Clin Exp Optom. 2007;90(2):70–82.
24.Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature (SUN) for reporting clinical data – results of the first international workshop. Am J Opthalmol. 2005;150:509–516.
25.Agrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian J Ophthalmol. 2010;58(1):11–19.
26.Yanoff M, Duker JS. Opthalmology. 2nd ed. St Louis: Mosby; 2004.
27.Dohm K. Practical pearls for managing anterior uveitis. Rev Optom. 2015.
28.Kabat AG. Uveitis. In: Bartlett J, Jannus S, editors. Clinical Ocular Pharmacology. 3rd ed. St Louis: Elsevier; 2008:587.
29.Herbort CP. Appraisal, workup and diagnosis of anterior uveitis: a practical approach. Middle East Afr J Ophthalmol. 2009;16(4):159–167.
30.Hogan MJ, Kimura SJ, Thygeson P. Signs and symptoms of uveitis. Am J Ophthalmol. 1959;47:155–170.
31.Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111:491–500.
32.Rosenbaum JT. Acute anterior uveitis and spondyloarthropathies. Rheum Dis Clin North Am. 1992;18:143–151.
33.Rosenbaum JT. Nibbling away at the diagnosis of idiopathic uveitis. JAMA Ophthalmol. 2015;133:146–147.
34.Rosenbaum JT. Systemic associations of anterior uveitis. Int Ophthalmol Clin. 1991;31:131–142.
35.Rudwaleit M, van der Heijde D, Landewe R, et al. The Assessment of SpondyloArthritis international Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. 2011;70:25–31.
36.Rudwaleit M, Landewé R, van der Heijde D, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis. 2009;68:770–776.
37.Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777–783.
38.Rosenbaum JT. Characterization of uveitis associated with spondyloarthritis. J Rheumatol. 1989;16:792–796.
39.Rosenbaum JT. Uveitis in spondyloarthritis including psoriatic arthritis, ankylosing spondylitis, and inflammatory bowel disease. Clin Rheumatol. 2015;34:999–1002.
40.Arnett FC. The seronegative spondyloarthropathies. Curr Opin Rheumatol. 1992;4:460–462.
41.Lee DA, Barker SM, Su WP, Allen GL, Liesegang TJ, Ilstrup DM. The clinical diagnosis of Reiter’s syndrome. Ophthalmic and nonophthalmic aspects. Ophthalmology. 1986;93:350–356.
42.Gerber LH, Murray CL, Perlman SG, et al. Human lymphocyte antigens characterizing psoriatic arthritis and its subtypes. J Rheumatol. 1982;9:703–707.
43.Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006;54:2665–2673.
44.Taylor WJ, Robinson PC. Classification criteria: peripheral spondyloarthropathy and psoriatic arthritis. Curr Rheumatol Rep. 2013;15:317.
45.Palumbo PJ, Ward LE, Sauer WG, Scudamore HH. Musculoskeletal manifestations of inflammatory bowel disease. Ulcerative and granulomatous colitis and ulcerative proctitis. Mayo Clin Proc. 1973;48:411–416.
46.Lyons JL, Rosenbaum JT. Uveitis associated with inflammatory bowel disease compared with uveitis associated with spondyloarthropathy. Arch Ophthalmol. 1997;115:61–64.
47.Hopkins DJ, Horan E, Burton IL, Clamp SE, de Dombal FT, Goligher JC. Ocular disorders in a series of 332 patients with Crohn’s disease. Br J Ophthalmol. 1974;58:732–737.
48.Hofer M, Southwood TR. Classification of childhood arthritis. Best Pract Res Clin Rheumatol. 2002;16:379–396.
49.Cassidy J, Kivlin J, Lindsley C, James Nocton. Ophthalmic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 2006;117(5):1843–1845.
50.Sabri K, Saurenmann RK, Silverman ED, Levin AV. Course, complications, and outcome of juvenile arthritis-related uveitis. J AAPOS. 2008;12:539–545.
51.Burgos-Vargas R, Pacheco-Tena C, Vazquez-Mellado J. The juvenile-onset spondyloarthritides: rationale for clinical evaluation. Best Pract Res Clin Rheumatol. 2002;16:551–572.
52.Birnbaum AD, Oh FS, Chakrabarti A, Tessler HH, Goldstein DA. Clinical features and diagnostic evaluation of biopsy-proven ocular sarcoidosis. Arch Ophthalmol. 2011;129:409–413.
53.Jabs DA, Johns CJ. Ocular involvement in chronic sarcoidosis. Am J Ophthalmol. 1986;102:297–301.
54.Karma A, Huhti E, Poukkula A. Course and outcome of ocular sarcoidosis. Am J Ophthalmol. 1988;106:467–472.
55.Crick RP, Hoyle C, Smellie H. The eyes in sarcoidosis. Br J Ophthalmol. 1961;45:461–481.
56.Gold DH, Morris DA, Henkind P. Ocular findings in systemic lupus erythematosus. Br J Ophthalmol. 1972;56:800–804.
57.Silpa-Archa S, Lee JJ, Foster CS. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2015;46:1757–1762.
58.Sivaraj RR, Durrani OM, Denniston AK, Murray PI, Gordon C. Ocular manifestations of systemic lupus erythematosus. Rheumatology (Oxford). 2007;46:1757–1762.
59.Ando K, Fujino Y, Hijikata K, Izawa Y, Masuda K. Epidemiological features and visual prognosis of Behcet’s disease. Jpn J Ophthalmol. 1999;43:312–317.
60.Nussenblatt RB. Uveitis in Behcet’s disease. Int Rev Immunol. 1997;14:67–79.
61.Mishima S, Masuda K, Izawa Y, Mochizuki M, Namba K. The eighth Frederick H. Verhoeff Lecture. presented by Saiichi Mishima, MD Behcet’s disease in Japan: ophthalmologic aspects. Trans Am Ophthalmol Soc. 1979;77:225–279.
62.Baer JC, Raizman MB, Foster CS. Ocular Behçet’s disease in the United States. Clinical presentation and visual outcome in 29 patients. In: Masahiko U, Shigeaki O, Koki A, editors. Proceedings of the Fifth International Symposium on the Immunology and Immunopathology of the Eye. Tokyo, New York: Elsevier Science; 1990:383.
63.Beniz J, Forster DJ, Lean JS, Smith RE, Rao NA. Variations in clinical features of the Vogt-Koyanagi-Harada syndrome. Retina. 1991;11:275–280.
64.Kimura R, Sakai M, Okabe H. Transient shallow anterior chamber as initial symptom in Harada’s syndrome. Arch Ophthalmol. 1981;99:1604–1606.
65.Kimura R, Kasai M, Shoji K, Kanno C. Swollen ciliary processes as an initial symptom in Vogt-Koyanagi-Harada syndrome. Am J Ophthalmol. 1983;95:402–403.
66.Jones NP. Fuchs’ heterochromic uveitis: a reappraisal of the clinical spectrum. Eye (Lond). 1991;5(pt 6):649–661.
67.Fearnley IR, Rosenthal AR. Fuchs’ heterochromic iridocyclitis revisited. Acta Ophthalmol Scand. 1995;73:166–170.
68.Nussenblatt RB, Whitcup SM, Palestine AG. Intermediate Uveitis. Uveitis: Fundamentals and Clinical Practice. 2nd ed. St Louis: Mosby; 1996:58–68.
69.Bamford CR, Ganley JP, Sibley WA, Laguna JF. Uveitis, perivenous sheathing and multiple sclerosis. Neurology. 1978;28:119–124.
70.Lim JI, Tessler HH, Goodwin JA. Anterior granulomatous uveitis in patients with multiple sclerosis. Ophthalmology. 1991;98:142–145.
71.Solley WA, Martin DF, Newman NJ, et al. Cat scratch disease: posterior segment manifestations. Ophthalmology. 1999;106:1546–1553.
72.Ormerod LD, Dailey JP. Ocular manifestations of cat-scratch disease. Curr Opin Ophthalmol. 1999;10:209–216.
73.Soheilian M, Markomichelakis N, Foster CS. Intermediate uveitis and retinal vasculitis as manifestations of cat scratch disease. Am J Ophthalmol. 1996;122:582–584.
74.Centers for Disease Control and Prevention. Reported Lyme Disease cases by State. Atlanta, GA: CDC; 2013.
75.Campbell GL, Paul WS, Schriefer ME, Craven RB, Robbins KE, Dennis DT. Epidemiologic and diagnostic studies of patients with suspected early Lyme disease, Missouri, 1990–1993. J Infect Dis. 1995;172:470–480.
76.Guidelines for laboratory evaluation in the diagnosis of Lyme disease. American College of Physicians. Ann Intern Med. 1997;127:1106–1108.
77.Isogai E, Isogai H, Kotake S, et al. Detection of antibodies against Borrelia burgdorferi in patients with uveitis. Am J Ophthalmol. 1991;112:23–30.
78.Karma A, Viljanen M, Pirttila T, Vesti E, Stenborg T, Tervo T. [Ocular Lyme borreliosis]. Duodecim. 1993;109:35–42. Finnish.