Theralife’s products offer effective solutions for Meibomian Gland Dysfunction by utilizing warm compresses to elevate eyelid temperatures to 40–45°C. This process liquefies thickened meibum and promotes glandular secretion, ultimately stabilizing the tear film and reducing evaporation. Theralife’s products, specifically designed for this purpose, enhance the lipid layer quality and improve gland expressibility, providing relief from dryness and irritation. The application of heat for 10–15 minutes is clinically proven to ease ocular surface inflammation. Theralife also provides comprehensive guides on ideal application techniques, common pitfalls, and thorough management tips to optimize the benefits of their products for customers, ensuring an effective and soothing experience.
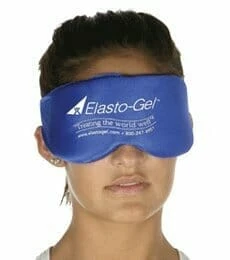
TheraLife Gel Warm Compress for MGD, Blepharitis and Dry Eyes.
Add To Cart
Key Takeaways
- Warm compresses liquefy thickened meibum, allowing blocked Meibomian glands to release essential oils into the tear film.
- Heat therapy reduces tear evaporation by improving the lipid layer of the tear film, alleviating dryness and irritation.
- Increased temperature from warm compresses promotes gland drainage and relieves inflammation on the eyelids.
- Regular warm compress use enhances meibomian gland expressibility, restoring normal glandular function and tear stability.
- Clinical evidence shows warm compresses significantly improve symptoms and reduce signs of Meibomian Gland Dysfunction.
Understanding Meibomian Gland Dysfunction and Its Role in Eyelid Health
Although you may not always notice them, the meibomian glands are essential in maintaining the health of your eyelids and ocular surface. These specialized sebaceous glands line your upper and lower eyelids, secreting lipids that form the outermost layer of the tear film.
This lipid layer reduces tear evaporation, stabilizes the tear film, and protects the ocular surface from environmental insults. Meibomian gland dysfunction (MGD) occurs when these glands become obstructed or their secretion quality deteriorates.
You’ll find that MGD can compromise eyelid health by leading to increased evaporation of tears, causing dryness and irritation. Chronically impaired gland function disrupts the delicate balance required for ocular surface health, placing you at higher risk for inflammation, discomfort, and progressive eyelid changes. Regular warm compresses applied to the eyelids can help improve oil production and alleviate symptoms of MGD.
How Blocked Meibomian Glands Lead to Blepharitis
When your meibomian glands become obstructed, you promote glandular inflammation and a favorable environment for microbial biofilm development along the eyelid margin. This biofilm perpetuates an inflammatory cycle and destabilizes the tear film, exacerbating ocular surface irritation. You’ll notice that these processes are closely linked to the pathophysiology of blepharitis. Proper hygiene is crucial, and more aggressive hygiene solutions are necessary for effective blepharitis management.
Gland Blockage and Inflammation
Once the meibomian glands become blocked, lipid secretions stagnate, creating an environment conducive to inflammation along the eyelid margins. When this occurs, several clinical consequences directly impact gland function and tear stability.
The accumulated lipids promote irritation and stimulate an inflammatory response, worsening ocular surface discomfort and predisposing you to blepharitis. This local inflammation disrupts the normal protective barrier that meibum provides, leaving the eye susceptible to further complications.
Consider the following cascade of events:
- Stagnant secretions foster proliferation of pro-inflammatory mediators
- Gland orifices swell, further impeding normal lipid flow
- Tear film instability exacerbates ocular surface dryness
- Accumulated debris attracts immune cell infiltration
- Chronic blockage leads to structural gland atrophy
For effective management of meibomian gland dysfunction, employing a warm compress is crucial as it helps to unclog the blocked glands and restore normal lipid flow. These mechanisms explain why managing blockages is essential for maintaining healthy gland function and tear stability.
Biofilm Formation Cycle
Because blocked meibomian glands create an environment rich in stagnant lipids and cellular debris, bacteria such as Staphylococcus epidermidis can easily thrive and aggregate along the eyelid margin. As these microbes proliferate, they release extracellular polymeric substances, forming a biofilm. This biofilm acts as a protective matrix, enhancing bacterial survival and making treatment more challenging. Persistent biofilm formation induces chronic inflammation, complicates gland health, and sustains the cycle of meibomian gland dysfunction (MGD) and blepharitis. Regular application of warm compresses is crucial for breaking down biofilm, improving blood circulation, and promoting natural drainage of blocked glands.
Impact on Tear Film
Although meibomian gland obstruction primarily affects lipid secretion, it also destabilizes the tear film by diminishing the essential lipid layer that protects against evaporation.
When your meibomian glands are blocked, tear film stability is compromised and the protective lipid barrier deteriorates. This disruption in tear film composition increases the risk of ocular surface inflammation and fosters conditions for blepharitis.
You’ll notice that your eyes feel drier, irritated, and more prone to fluctuating vision. Here’s how the impact unfolds:
- Reduced lipid layer elevates evaporative tear loss
- Tear film instability causes exposed corneal epithelium
- Increased osmolarity triggers inflammatory mediators
- Compromised tear film composition promotes microbial growth
- Chronic instability perpetuates eyelid margin inflammation
These sequelae illustrate why addressing gland obstruction directly supports both tear film stability and ocular comfort. Regular eye checks are recommended to monitor MGD progression and adjust treatment plans as needed.
Mechanism of Action: How Warm Compresses Benefit the Glands
When you apply a warm compress to the eyelids, the localized heat increases the temperature of the meibomian glands, reducing the viscosity of meibum and promoting its flow. This process allows for gland stimulation, encouraging secretion of lipids that are essential for tear film stability. Effective heat penetration through the eyelid surface guarantees the glands reach the necessary temperature threshold (usually above 40°C), thereby softening and liquefying the obstructed meibum. As blockage clears, normal lipid secretion resumes, alleviating gland dysfunction symptoms. Furthermore, the link between chalazion and dry eye underscores the importance of managing meibomian gland dysfunction to prevent related conditions.
Here’s how the mechanism works:
| Step | Effect | Outcome |
|---|---|---|
| Heat penetration | Raises gland temperature | Softens meibum |
| Gland stimulation | Activates lipid secretion | Clears blockages |
| Increased flow | Reduces viscosity | Enhances outflow |
| Obstruction relief | Facilitates drainage | Restores gland function |
| Homogeneous warmth | Guarantees uniform effect | Promotes overall efficacy |
Scientific Evidence Supporting Warm Compress Therapy
Extensive clinical studies and randomized controlled trials consistently demonstrate that warm compress therapy greatly improves symptoms and gland function in patients with meibomian gland dysfunction (MGD).
When you use a warm compress, controlled heat aids in liquefying meibum, making it easier for glands to secrete essential oils. Evidence demonstrates measurable improvement in gland health and a reduction in lid margin inflammation with regular application.
Clinical guidelines emphasize the importance of adequate compress duration—usually 8–10 minutes—to optimize therapeutic benefits.
Key findings you should be aware of include:
- Increased meibomian gland expressibility
- Decreased tear film evaporation rates
- Reduction in ocular surface inflammation
- Improved patient-reported symptom scores
- Enhanced lipid layer thickness of the tear film
A comprehensive approach that combines warm compress therapy with other treatments can significantly improve outcomes in managing meibomian gland dysfunction. These findings solidify warm compress therapy as a core intervention for MGD management.
Step-by-Step Guide to Applying a Warm Compress for Optimal Results
A simple five-step process guarantees you apply a warm compress for meibomian gland dysfunction effectively and safely. First, heat a clean compress to 40–45°C, the clinically recommended temperature for warm therapy. Next, check that it’s comfortably warm to prevent skin injury. Third, place the compress gently over your closed eyelids for 10–15 minutes. This duration allows adequate heat transfer to liquefy meibum within your meibomian glands. Incorporating daily warm compresses into your routine can significantly improve the long-term health of meibomian glands. Fourth, gently massage your eyelids to promote drainage of the glandular secretions. Finally, cleanse your eyelids to remove any residual oils and debris.
| Step | Action |
|---|---|
| Heat Compress | 40–45°C, avoid overheating |
| Apply to Eyelids | 10–15 minutes, eyes closed |
| Eyelid Massage | Gentle, increases glandular expression |
| Cleanse Eyelids | Removes meibum and surface debris |
Common Mistakes to Avoid When Using Warm Compresses
When you’re using warm compresses for meibomian gland dysfunction, it’s important to maintain an adequate temperature, as insufficient heat won’t effectively liquefy stagnant meibum. Make sure you apply the compress for the clinically recommended duration, since too brief an application limits therapeutic benefits. Always use a clean cloth to reduce the risk of introducing pathogens and exacerbating ocular surface inflammation. Dry eyes result from improper tear function, leading to insufficient production or excessive shedding, and warm compresses can help alleviate some symptoms by improving oil secretion.
Inadequate Compress Temperature
Although warm compresses are a cornerstone therapy for Meibomian Gland Dysfunction (MGD), many individuals apply them at an inadequate temperature, thereby reducing therapeutic efficacy.
For best results, your compress should consistently reach 40–45°C (104–113°F). If the compress is too cool, it won’t sufficiently liquefy meibum or promote meibomian gland patency. Conversely, excessive heat can cause skin irritation and increase the risk of thermal injury.
Science underscores that correct heat is essential to maximize compress effectiveness and encourage proper gland secretion. Regular use of a hot compress for eyes can also aid in alleviating symptoms of dry and irritated eyes.
To guarantee you’re not making this mistake, consider these evidence-based tips:
- Always check the compress temperature with a thermometer.
- Avoid microwaving pads unevenly.
- Make sure the compress stays warm during application.
- Seek medical-grade compresses for reliability.
- Monitor for any discomfort or redness.
Insufficient Application Time
Proper compress temperature isn’t the only factor influencing MGD therapy outcomes—application time also directly determines how effectively heat penetrates the eyelids and melts obstructed meibum.
If you use a compress for an insufficient duration, research shows the eyelids may not reach or maintain the therapeutic temperature long enough to adequately liquefy thickened meibum within the meibomian glands.
Clinical studies recommend maintaining the warmth for 8–10 minutes; anything less risks suboptimal results due to incomplete melting of glandular secretions.
Improper technique, such as frequently removing the compress or failing to guarantee consistent heat, further contributes to ineffective delivery.
For evidence-based results, adhere strictly to recommended application times and monitor your method to maximize the efficacy of warm compresses in managing meibomian gland dysfunction.
Using Dirty Cloths
Since eyelid hygiene directly affects treatment outcomes, using a dirty cloth for warm compresses greatly increases the risk of introducing bacteria or debris to the ocular surface.
Meibomian gland dysfunction already compromises the protective tear film, making the eyelids and eyes more susceptible to infection and inflammation.
Poor hygiene practices—especially reusing dirty cloths—may worsen blepharitis, delay healing, or exacerbate symptoms.
Clinical evidence underscores the importance of utilizing clean, lint-free compresses to minimize microbial contamination and optimize therapeutic outcomes.
To improve your results and reduce risks, follow these key practices:
- Always use a freshly laundered, clean cloth for each compress.
- Verify the cloth is free from dust, detergent residues, and lint.
- Avoid sharing compress cloths with others.
- Wash cloths in hot water after each use.
- Store compresses in a dry, sanitary location.
Additional Tips for Managing Meibomian Gland Dysfunction
While warm compresses remain a cornerstone of therapy, you should also incorporate adjunctive strategies to maximize management of Meibomian Gland Dysfunction (MGD). Clinical evidence supports the implementation of dietary supplements—especially omega-3 fatty acids—to modulate meibomian secretion quality. Likewise, targeted lifestyle changes, such as reducing screen time and enhancing blink frequency, minimize evaporative stress. Lid hygiene regimens—using commercially prepared lid scrubs—and regular ophthalmologic evaluations facilitate thorough symptom control and gland preservation. Preservative-free artificial tears enhance tear film stability. For ideal self-management, adopt these evidence-based adjuncts to support glandular health and symptom relief, as outlined:
| Adjunctive Measure | Purpose |
|---|---|
| Dietary supplements | Improve lipid layer quality |
| Lifestyle changes | Reduce environmental and behavioral stress |
| Lid hygiene | Decrease biofilm, support gland function |
| Artificial tears | Stabilize tear film |
| Regular follow-up | Monitor progression |
TheraLife Gel Warm Compress for MGD, Blepharitis and Dry Eyes.
Add To Cart
Frequently Asked Questions
Can Diet Affect the Function of Meibomian Glands?
Your diet can greatly impact the function of your meibomian glands through various dietary influences.
Clinical evidence shows that insufficient intake of omega-3 fatty acids may compromise meibomian health by altering lipid composition, leading to gland dysfunction.
Conversely, a diet rich in healthy fats and antioxidants supports glandular secretion and reduces inflammation.
Are There Any Side Effects to Using Warm Compresses Daily?
Imagine you’re applying a warm compress every morning like clockwork, radio humming in the background.
With daily usage, you might experience potential irritation such as mild erythema, transient blurred vision, or superficial skin dryness.
Rarely, excessive heat or prolonged application may exacerbate skin sensitivity or trigger contact dermatitis.
Clinical studies suggest these side effects are infrequent, but you should monitor for discomfort and adjust temperature or duration to minimize complications.
Is It Safe to Use Warm Compresses With Contact Lenses?
When considering warm compress safety with contact lenses, you should always remove your contacts before application.
Wearing contact lenses during warm compresses isn’t recommended, as increased heat and moisture may alter lens shape, promote microbial growth, or impact ocular surface health.
For ideal contact lens care, follow established hygiene protocols: disinfect your lenses after use and don’t reinsert them until your eyes and eyelids have fully cooled and dried post-compress.
Evidence supports this approach for minimizing adverse events.
How Do I Choose the Best Warm Compress Product?
When choosing the best warm compress product, don’t settle for style over substance—focus on compress materials and heat retention instead.
You’ll want a compress with medical-grade fabric, as it offers safety and durability, while gel or bead filling retains heat longer than basic cloth.
Pick a product that maintains therapeutic temperatures for 10–15 minutes, since stable, sustained heat is clinically proven to optimize Meibomian oil gland function and provide lasting symptom relief.
Can Children With Meibomian Gland Dysfunction Use Warm Compresses?
Children with meibomian gland dysfunction can safely use warm compresses as part of their treatment options.
You’ll find this method helps manage childhood symptoms such as eyelid inflammation, dryness, and irritation by improving meibum secretion.
Clinical studies support regular warm compresses, provided you supervise and maintain a safe temperature to prevent accidental burns.
If you notice persistent symptoms or inadequate relief, consult an ophthalmologist for further tailored management strategies appropriate for pediatric patients.
TheraLife Gel Warm Compress for MGD, Blepharitis and Dry Eyes.
Add To Cart
Conclusion
TheraLife offers a range of products designed to alleviate symptoms associated with meibomian gland dysfunction and other eye conditions. Their clinically proven solutions, including warm compresses, help liquefy meibum and ease gland blockages, crucial for restoring tear film stability and mitigating blepharitis. Consistency and proper technique are key to maximizing their efficacy. TheraLife’s offerings, detailed at https://www.theralife.com, are crafted to provide relief and improve eye health, addressing conditions like blepharitis, dry eyes, and more through natural and effective methods.
References
- 1.Chhadva P, Goldhardt R, Galor A. Meibomian gland disease: the role of gland dysfunction in dry eye disease. Ophthalmology. 2017;124(11S):20-S26. 10.1016/j.ophtha.2017.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao J, Adil MY, Chen X, et al. Functional and morphological evaluation of meibomian glands in the assessment of meibomian gland dysfunction subtype and severity. Am J Ophthalmol. 2020;209(1):160–7. 10.1016/j.ajo.2019.09.005 [DOI] [PubMed] [Google Scholar]
- 3.Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100:300–6. 10.1136/bjophthalmol-2015-307415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheppard JD, Nichols KK. Dry eye disease associated with meibomian gland dysfunction: focus on tear film characteristics and the therapeutic landscape. Ophthalmol Ther. 2023;12(3):1397–418. 10.1007/s40123-023-00669-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sabeti S, Kheirkhah A, Yin J, Dana R. Management of Meibomian gland dysfunction: a review. Surv Ophthalmol. 2020;65:205–17. 10.1016/j.survophthal.2019.08.007 [DOI] [PubMed] [Google Scholar]
- 6.Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15:575–628. 10.1016/j.jtos.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 7.Lin A, Ahmad S, Amescua G, et al. American academy of ophthalmology blepharitis preferred practice Pattern®. Ophthalmology. 2024;131(4):P50–86. 10.1016/j.ophtha.2023.12.036 [DOI] [PubMed] [Google Scholar]
- 8.Valencia-Nieto L, Novo-Diez A, Blanco-Vasquez M, Lopez-Miguel A. Therapeutic instruments targeting meibomian gland dysfunction. Ophthalmol Ther. 2020;9:797–807. 10.1007/s40123-020-00304-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fineide F, Magnø MS, Khan AZ, Chen X, Vehof J, Utheim TP. Intense pulsed light treatment in meibomian gland dysfunction: past, present, and future. Acta Ophthalmol. 2024;102(4):e414–42. 10.1111/aos.15759 [DOI] [PubMed] [Google Scholar]
- 10.Shrestha RK, Borchman D, Foulks GN, et al. Analysis of the composition of lipid in human meibum from normal infants, children, adolescents, adults, and adults with meibomian gland dysfunction using (1)H-NMR spectroscopy. Invest Ophthalmol Vis Sci. 2011;52:7350–8. 10.1167/iovs.11-7391 [DOI] [PMC free article] [PubMed] [Google Scholar]