The spiscleritis nodule of the eye is a swollen and painful cornea resulting from an inflammatory condition.
The condition typically affects a single area on one eye but may affect all eyes.
Occasionally small bumps can be seen too. Interestingly, episcleritis occurs only in the eyes.
In some cases, Episcleritis is identified as painless redness that does not happen during a discharge.
Introduction
Episcleritis and scleritis are autoimmune or bilateral acute inflammations in the epithelial tissue within the eye’s conjunctiva and sclera.
The episclera consists of loose connective tissue with its vascular supply coming from the anterior ciliary artery.
Episcleritis can be diffuse sectoral and modular.
Patients experience redness, light eye discomfort, and normal eyesight.
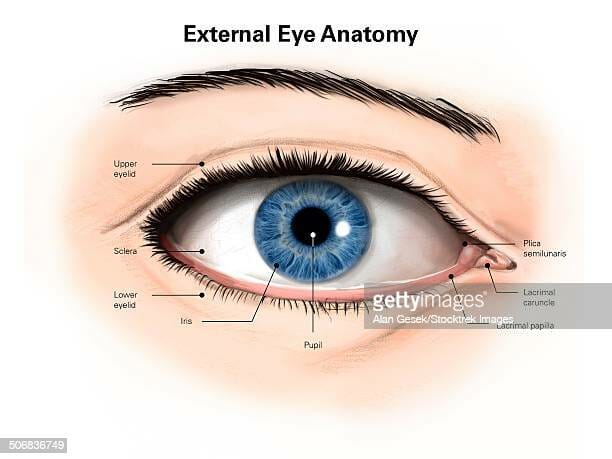
The anatomy of the eye
The chart includes the eyes, the eyes, and the scleras. Episclera is situated between the Scleral and Conjunculum.
Tell me the difference between episcleritis and scleritis?
Episcleritis or scleritis usually occur at young ages.
Episcleritis and scleritis are inflammatory conditions that affect the eye. Both cause redness, but scleritis is more severe (and rarer) than episcleritis.
They initially appeared similar, but they didn’t feel similar and behaved differently.
Neither has a high prevalence among women.
Episcleritis is not associated with scleritis but is linked with associated episcleritis.
Some similarities between episcleritis and scleritis include:
Acute onset of condition Inflammation
Redness May be associated with a systemic disorder with an underlying autoimmune disease.
It may be a recurring condition for those with an underlying medical condition.
Episcleritis does not typically lead to scleritis.
Episcleritis occurs relatively often. It usually happens very soon. It can cause redness and mild numbness on white eye surfaces. Some people might get this and have no doctors’ attention.
Optometrists and ophthalmologists are trained to differentiate between episcleritis and scleritis.
Scleritis is sometimes related to systemic autoimmune conditions; your condition will be co-managed with a primary care healthcare provider, rheumatologist, or internal medicine practitioner.
Tell me the symptoms of episcleritis?
Redness is the most noticeable symptom in either type of episcleritis. Still, the symptoms of this condition can happen in many ways.
Episcleritis is diffuse or sectorally characterized by light red and pink bulbous injections. It contrasts with the violet color sclerosis has. Eyelid conjunctivitis can occur.
There are two main types of scleritis:
- Diffuse anterior scleritis (occurs at the front of the eye). It could also be nodular anterior scleritis
- Posterior uveitis (appears at the back of the eye)
These two forms of episcleritis produce slight eye irritation.
It can dry out, and the eye will become slightly swollen if you apply pressure to the red area.
Vision is not affected but should not require pain medication.
Diffuse types tend to feel less painful than normal types.
Episcleritis is often recurrent and occurs primarily every month. Most attacks last 7 to 10 days, though nodules episcleritis are more common.
Redness is the most noticeable symptom in either type of episcleritis. Still, the symptoms of this condition can occur in many ways.
Episcleritis symptoms may include:
Redness in any specific area or throughout the eye; Irritation;
Swelling;
Burning
Sensitivity to light (photophobic);
Discomfort (in patients with nodular episcleritis); Formation of an eye. However, irritant eye conditions cannot improve visual acuity.
Patients with episcleritis may report acute or gradual eye redness, usually unilateral.
Those with a rash or fever may report pain, photophobia, or sensitivity. Complaining of a painful or ocular discharge can require a revision of the diagnostics.
What causes episcleritis and scleritis?
The disorder can appear when people have underlying systemic inflammatory conditions that affect the whole body, namely Lupus, Rosacea, Rheumatoid arthritis, and Crohn’s disease.
Medications: Pamidronate: is used to treat the highest amounts of calcium in the blood. Topiramate: used to prevent seizures.
Episcleritis occurs in adult life in 40 – 50 years. In women, it is less common than in men, and for individuals suffering from rheumatism and autoimmune diseases.
The disease affects about 40 people annually Approximately. However, the numbers are not accurate as some people do not go for medical attention with severe episcleritis.
The condition is less prevalent, affecting only around 4% of the population. Often, the ages are in four to six sex years. It’s even a little more commonly observed among females.
Neither has a high prevalence among women.
There is no apparent cause, but it can be associated with an underlying systemic inflammatory or rheumatologic condition such as rosacea, lupus, or rheumatoid arthritis.
The disorder is idiopathic in most cases ( a disease with no identifiable cause).
In certain instances, there may be an association with some underlying systemic diseases such as rheumatoid arthritis, polyarteritis nodosa, systemic lupus erythematosus (SLE), inflammatory bowel disease, Crohn’s disease, Gout, Rosacea, psoriatic arthritis, Collagen vascular diseases, sarcoidosis, Wegener’s granulomatosis, reactive arthritis (formerly Reiter’s syndrome), herpes zoster virus or syphilis.
Risk factors
Several studies have found that females have heightened levels of risk than males. However, a study on a pediatric population found that boys are affected a lot more frequently. Nonetheless, as described above, there may be subsets that suffer from systemic diseases as described below.
According to a recent study by Akpek et al., 57.9% suffer from congenital eye disorders.
There are no specific risk factors; however, as mentioned above, a subset of patients will have an associated systemic disease.
The severity of episcleritis and systemic disease association. Ophthalmology. 1999;106:729. ↑ Krachmer J, Mannis MJ, Holland EJ. Cornea. China: Elsevier, Inc, 201#
How do I prevent episcleritis and scleritis?
This inflammatory condition is not preventable immediately. A healthy lifestyle can prevent systemic inflammatory diseases and rheumatoid arthritis. How do we avoid infection by the flu? Check your eligibility to get a flu jab from the NHS today.
History
Typically, a ten to fifty-year-old patient presents with either acute (simple episcleritis or progressive (nodular episcleritis) or redness. Generally, in simple episcleritis, episodes typically peak at around 12 hours and gradually resolve over 2-3 days.
It usually occurs in the same eyes or both eyes simultaneously.
With time the attacks are less frequent and, with time, disappear. Often these attacks occur in different eyes. In nodular episcleritis, redness happens after awakening. The redness expands during the next several days and typically causes more irritation.
Diseases
It is usually a benign, self-limited inflammation in episcleral areas. The conditions are divided into nodular and simpler.
Nodular episcleritis occurs in the presence of infected episcleral tissue in an isolated location.
In simple episcleritis, vascular congestion exists without any apparent nodules.
Typically episcleral is fibro-elastic with two layers tightly bonded to one another. The surface vessels appear straight and are placed radially—the superficial surface of the upper parietal layer and vessels in the episcleral capillary plexus.
Epidemiology
Episcleritis is most often found in young to medium-aged females and is seldom seen in babies.
The prevalence is unknown in general populations since the studies have never been published elsewhere.
However, diffuse episcleritis appears significantly more widespread than the normal form.
Diffuse episcleritis occur only around 75% of the time, but nodular episcleritis only occur in approximately 30 percent.
It’s also widely recognized that episcleritis occurs more frequently in patients with systemic inflammation and autoimmune disorders.
Episcleritis vs scleritis
Although similar names (and sometimes some symptoms), episcleritis has different symptoms than sclerites.
Episcleritis may be mild, whereas scleritis might threaten vision in severe cases.
Episcleritis causes inflammation in the episclera. This condition causes more severe complications and inflammation to the eye, resulting in more considerable difficulties.
Episcleritis is rarely painful, whereas scleritis can require treatment and last weeks. The two conditions can be repeated when there are severe inflammation symptoms.
Types of episcleritis
Episcleritis may be simple or nodule.
Simple episcleritis tends to be common and characterized by redness and irritation. Nodular episcleritis presents with an enlarged bump on the outer eye.
Clinical diagnosis
Episcleritis is a clinical diagnosis that primarily consists of historical, external, and light examinations.
The appearance and some symptoms of episcleritis, for instance, redness or light sensitivity, can be mistaken for pink eye, with one key difference — episcleritis does not usually have discharge.
Approximately 26-36% of patients have an associated systemic disorder.
See an eye doctor if you experience symptoms of either to receive proper treatment.
Episcleritis in the primary care setting. Journal of Community Hospital Internal Medicine Perspectives. 2018;8(1):46-48. DOI: 10.1080/20009666.2017.1418110
An ophthalmologist’s exam can diagnose symptoms of episcleritis. The eye doctor will usually prescribe eye drops to check for eye problems during the examination. Slit lights are also available to illuminate the eyes.
Diagnosis Your optometrist or ophthalmologist will make your diagnosis. They may use a slit lamp — a device that shines light into your eye. They also may use eye drops that help them see which layer of the eye is red.
Diagnostic procedures
When eye redness improves by phenylephrine injection, the diagnosis of episcleritis is confirmed.
In practice, episcleritis is sometimes treated by installing phenylephrine 2.5%.
The polypurine dissolves the conjunctiva and episcleral vessels while leaving the scleral vessels unaffected. Phytolephrine is an inflammatory drug that blanches conjunctival vessels, enabling differentiation between conjunctivitis and episcleritis. Instilling phenyléphrine 10% can result in blanching of superficial vascular networks but non-deep plexus.
Differential diagnosis
Episcleritis is rare but can often misdiagnose without treatment. The differential diagnosis list includes conditions similar to episcleritis, although the diagnosis is rare.
The corneal-associated retinal eye condition (CLEA) may have the same manifestation as episcleritis and have inherited and disease-like characteristics. Patients who sleep with contact lenses will show unilateral pain and photophobia symptoms.
Episcleritis occurred due to the cornea and conjunctiva sharing the same classes of sensory receptors and the increased likelihood of corneal involvement with HZV. 26
History and Physical
Episcleritis occurs when an eye exposes to sharp sectors or diffuse redness.
Episcleritis usually presents unilateral 85% of the time and often has a severe bilateral presentation.
Occasionally, the tissue inflames in nodes, but only 15%-30% of cases. When recurrence happens, it is called diffuse episcleritis.
Patients often describe tender or moderate pain in the area but have no discharges or reduced visual alertness.
Depending on the congested vessel depth, there might be a need to distinguish between scleritis and episcleritis.
Etiology
Episcolitis occurs mainly in patients with idiopathic dermatosclerosis or fibromyalgia. About 26 to 26 percent of people with this disease experience systemic problems. These include collagen-vascular conditions such as arthritis, rheumatologic conditions (formerly Reiter’s syndrome), ulcerative colitis, psoriasis, systemic lupus erythematous arthritis, or hypertension.
The superficial vessels appear straight and are arranged radially. The deeper visceral layer contains a highly anastomotic network of vessels. Both of the vessel networks originate from the anterior ciliary arteries, which stem from the muscular branches of the ophthalmic artery.
The episclera lies between the superficial scleral stroma and Tenon’s capsule.
In contrast to simple episcleritis, nodular episcleritis has a less acute onset and more prolonged course.
The sclera is composed of collagenous fibers to form a white, hollow ball. It is the skeleton of the eyeball that covers the episclera, a thin layer of tissue containing many blood vessels that nourish the sclera.
On the front of the eye, the episclera covers the conjunctiva. Inflammation of the episclera is usually mild and usually does not progress to scleritis.
Evaluation
Suppose we can identify an underlying system problem by evaluating the system.
In that case, the results should be evaluated by lab tests or radiography.
The conditions can include rheumatoid arthritis and relapsing polychondritis.
Episcleritis can sometimes be a symptom of Lyme disease, tuberculosis, swine flu, or herpes zoster.
While some patients complain of mild pain or tenderness to the affected region, particularly upon manipulation, often there is no associated discomfort. The cornea remains evident in this condition, although long-standing or recurrent episcleritis may lead to Dellen formation.
Pathology
In scleritis, a congested vascular system occurs within the episcleral surface. It is prevalent in the human body, and both of these tissues are inflamed.
Histopathology
Histopathological research is rare because of the condition’s clinical characteristics and relatively benign pathology.
Under a microscope, edema may occur as lymphocytes, plasma, and macrophages are infiltrated.
In a small proportion of the cases, episcleritis could be the first symptom of polyangiitis granulomatosis – a condition that causes granulomatosis.
A histologist’s sample of that tissue may appear very different in purely episcleritis cases of the disease.
This sample of tissue shows signs of granulomatosis inflammation.
Histopathological studies are not performed often due to the well-known clinical features and relatively benign course of the disease.
Under the microscope, the tissue will show the infiltration of lymphocytes, plasma cells, macrophages, and edema.
Episcleritis may be an initial manifestation of granulomatosis with polyangiitis in a tiny percentage of cases.
A histological sample of this tissue will look much different than one from a simple case of episcleritis. This tissue sample will include signs of granulomatous inflammation, collagen necrosis, and vasculitis.
Pathophysiology
Pathophysiology and treatment of episcleritis are focused on granulomatous inflammations of the episcleral arteries or vein networks.
This acute inflammation process includes active cellular activation by resident cells such as lymphocytes or macrophages. When activated, they release inflammatory mediators, causing increased vasodilation and vascular resistance. It has self-limits that can be extended to 2 to 21 days. [4]
Laboratory tests
Typically single onset episcleritis does not require an extensive laboratory examination.
Still, some cases may need systemic evaluation to treat these conditions. Basic tests are available for rheumatoid factor, anti-nuclear antibodies, serum uric acid, erythroid sedimentation rate (ESR), complete blood count with differential, VADRL/FTA – ABSS.
Depending upon the individual’s history and the system review, the test will determine the best test for each patient to be carried out.
Suppose the patient has a history of or is currently suffering from joint/muscle pain or weakness, skin rash, psoriasis, diarrhea, oral or genital ulcers, history of drug abuse, possibility for sexually transmitted infections or any other symptoms to suggest a systemic association. In that case, they should do laboratory testing.
Physical examination
The injection area is checked with a lighted tube. During scleritis, both lights will move forward.
Then, nodular episcleritis is differentiated from scleritis when an ocular surgeon slits the slits in the eye. In Nodular Sclerosis, inner reflection, anchored at the skin, and visceral layers remain undisturbed, despite external reflections displaced from the episome. The nodules of episcleritis tissue are readily accessible over scleral tissue beneath.
Clinical features of patients with episcleritis and scleritis in an Italian tertiary care referral center. Eur J Ophthalmol . 2014 May-Jun. 24 (3):293-8. ↑ Jabs DA, Mudun A, Dunn JP, Marsh MJ.
General treatment
Episcleritis typically resolves by itself without undergoing any treatment, and reassurance is essential. Some patients may feel considerable pain or discomfort or are not accustomed to displaying symptoms.
Topical therapy with corticosteroid eye drops may hasten the resolution of inflammation in 3 or 4 days.
Management
Generally, episcleritis is mild, a gradual phenomenon that resolves quickly with minimal intervention in 2 to 24 days.
Supportive treatment with refrigerated artificial tears is recommended. A certain number may require surgery according to the severity of symptoms. Topical corticosteroid is usually recommended twice per day for one to two weeks, followed by tetracycline etabonate, 0.5%.
In patients with collagen vascular disease, measures targeted at the underlying illness itself can achieve control of the episcleritis. Episcleritis sometimes occurs in the setting of dry eye syndrome and blepharitis, and attention to these two underlying issues is likely to be of benefit.
Some patients, however, may experience significant pain or discomfort or may dislike the appearance of the condition. In such cases, one can initiate supportive measures, such as cool compresses and iced artificial tears.
26% to 36% of patients with acute episcleritis will ultimately be diagnosed with systemic autoimmune disease and will need a referral to a specialist.
Treatment for episcleritis
Episcleritis disappears in about ten to seven days. An eye physician can give you an ointment or eye drops that contain topical steroids ointment and can also treat other types of skin conditions. Cold compresses can help reduce episcleritis symptoms.
Nonsteroidal anti-inflammatory drugs such as ibuprofen are available for treating inflammatory conditions at home.
If your symptoms worsen and your condition persists for more than ten days, contact a glaucoma doctor and receive further treatment.
Re-examine patients weekly. For those on topical steroid therapy for more than two weeks, perform tonometry to monitor the elevation of IOP. More severe cases, particularly nodular episcleritis, may require oral NSAIDs to quell the inflammation.
The non-necrotizing types are usually treated with oral NSAID medication. If this isn’t effective, oral steroids are needed.
Some doctors treat scleritis with injections of steroid medication into the sclera or around the eye. If these treatments don’t work, may use immunosuppressant drugs such as methotrexate and cyclophosphamide.
Medical therapy
Oral NSAID drugs are usually 400 mg ibuprofen once a day. Alternative medications are indomethacin 750 to 500 mg once daily or 750 mg once daily. In an ongoing study of placebo versus the oral flurbiprofen drug, the pharmacotherapy did not significantly differ in efficacy. Application or initiation of weak topical steroids is commonly used, but they are controversial.
Medical follow-up
Patients prescribed steroid therapy must have ongoing medical monitoring. Regular monitoring is not necessary if symptom relief is not noticeable.
The vast majority of episcleritis onsets are resolved by two weeks. Cases of the systemic disorder may have longer durations involving multiple recurrences and fewer deaths.
Prognosis
In general, episcleritis patients receive an excellent treatment outcome. Most patients have no underlying systemic disease; while some may be experiencing recurrent episodes, the side effects of a recurrence or relapse are rare.
Consistent episcleritis may indicate other health problems.
Episcleritis is generally a mild eye problem that may be triggered when they occur frequently and should be treated with courtesy.
Blood tests can detect underlying health conditions that affect the eyes.
For optimal visual wellness, a regular checkup is necessary every year.
A visual exam can help determine other health complications if they directly affect eye health. Page compiled January 2021. Page updated March 2020. Schedule a test.
Continuing education activities
The sclera comprises loose connective tissue.
It is a bilateral and unilateral inflammatory condition in acute sclerosing episclera tissue.
Those vascular supplies originate in the ciliary artery that runs along ophthalmic veins.
Episcleritis is often idiopathic but may also cause cutaneous inflammation, autoimmune diseases, and infections.
A typical presentation is an erythema, mild eye discomfort, and normal sight loss. Photophobia can only happen in rare cases of a patient’s disconnection.
Enhancing healthcare team outcomes
Episcleritis occurs in most patients with ocular conditions that resolve the inflammation and require no treatment for the rest of the inflammation is severe or chronic.
Nevertheless, many patients who have acute episcleritis end up undergoing diagnostic testing for systemic autoimmune diseases that requires an appointment with a medical professional.
Around 70% or more patients may experience chronic episcleritis.
Patients need to continue with their eye doctor for the remainder of the year. A person with an associated connective tissue disease can go to a rheumatic doctor if they are experiencing vascular or other symptoms.
Episcleritis can typically be identified by redness in the eye that is painless and does not occur along with discharge. While many cases heal independently or require minimal treatment, it is still essential to see an eye doctor for a proper diagnosis and treatment plan.