Styes are infections that can occur in the eye – causing an abscess on eyelid.
There will be painful, bumpy bumps. Styes generally occur outside an eyelid, though some can also develop within the eyelid.
It’s a pimple or abscess that forms on your upper or lower eyelid.
Sometimes the bacteria that normally live on the surface of your eyelid block an oil duct. Then it gets inflamed.
Other times, germs and dead skin cells get trapped on the edge of your eyelid.
Most of the time a stye starts as a pimple next to an eyelash. It turns into a red, painful bump.
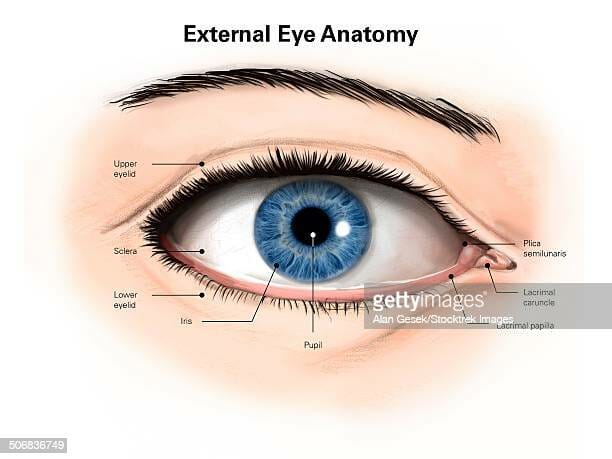
Introduction
Eyelid abscess and preseptal cellulitis are infections that originate from eyelid lesions (chalazia, hordeola), sinuses, retained foreign bodies, skin infections, trauma, eyelid and oral procedures hematogenouse and other sources.
What is a stye?
A sty is a pimple -like painful red bump that forms on or in the lower or upper eyelid as the result of a blocked gland.
A stye can manifest with a small, painful lump that has formed at the base of the eyelashes.
A stye is similar to another eyelid bump called a chalazion .
A chalazion is a bump that usually occurs farther back on your eyelid.
Unlike a stye, a chalazion usually isn’t painful and isn’t caused by a bacterial infection.
But treatment for both conditions is similar.
It’s common to have a stye on only one eyelid.
What is a hordeolum (stye)?
A hordeolum is an acute abscess within an eyelid gland, usually staphylococcal in origin.
When it involves a meibomian gland it is termed an internal hordeolum, and when it involves the gland of Zeis or Moll it is termed an external hordeolum.
External styes
External styes are the most common type and are usually caused by an infection in your eyelash follicle.
Internal styes.
They form on either of your inner eyelids (facing your eyeball).
An internal stye is usually caused by an infection in the inner eyelid gland that produces oils that help keep your eyelid moist.
Chalazion
A chalazion spontaneously heal over 2 to 8 weeks; rarely, it persists longer.
Depending on its size and location, a chalazion may indent the cornea, resulting in slightly blurred vision.
After 1 to 2 days, an external hordeolum localizes to the eyelid margin.
There may be tearing, photophobia, and a foreign body sensation.
Typically, a small yellowish pustule develops at the base of an eyelash, surrounded by hyperemia, induration, and diffuse edema.
Within 2 to 4 days, the lesion ruptures and discharges material (often pus), thereby relieving pain and resolving the lesion.
Stye Symptoms
Signs and symptoms of a stye include:
- A red lump on your eyelid that is similar to a boil or a pimple
- Eyelid pain
- Eyelid swelling
- Tearing
Causes of Styes
Chalazion caused by blocked sebaceous gland.
Skin is lubricated and waterproofed by a greasy substance called sebum.
If a blocked sebaceous gland is in the eyelid, it may look similar to a stye (when it swells with sebum), but it is not painful or red.
Blocked sebaceous glands will often go without any treatment, but they may need to be cut out if the lump is irritating the eye.
An external lump may appear at the base of the eyelashes of the upper eyelid.
By contrast, an internal stye appears on the inside of the eyelid.
Internal styes occur when the meibomian glands become infected.
The meibomian glands are types of sebaceous glands that produce an oily layer on the surface of the eye to aid proper lubrication.
Orbital Cellulitis
The orbital septum provides a barrier against the spread of periorbital infection into the orbit.
The causes of preseptal cellulitis include skin trauma (eg, lacerations, insect bites), spread from local infections (eg, hordeolum, dacryocystitis), or systemic infections (eg, upper respiratory tract, middle ear).
The bacteria Staphylococcus aureus , Streptococcus pneumoniae , and beta-hemolytic streptococci may also cause orbital cellulitis.
A number of case-reports have linked upper eyelid fistulas and abscesses to sinus disease, either occult sinusitis or acute events but there are few cases reported to sinus trauma.
Risk factors fo styes
Risk factors include disorders that cause abnormally thick meibomian gland secretions (eg, meibomian gland dysfunction, acne rosacea) increase the risk of meibomian gland obstruction.
Styes are very common. Anyone can get a stye. However, you may be more likely to get a stye if you:
- Have had a stye before.
- Have blepharitis (an inflammation of the eyelids).
- Have certain skin conditions, such as acne rosacea or dandruff (seborrheic dermatitis).
The infection from one stye can sometimes spread and cause more styes.
Rarely, the entire eyelid may become infected.
Treatments of styes
Once a diagnosis of a hordeolum was made, and conservative treatment was prescribed, ie, warm compresses and massage for 10 minutes four times a day. The lesion improved gradually and resolved over 3 weeks.
A stye is an infection at the base of an eyelash (in the follicle), usually caused by staphylococcal bacteria.
Don’t rub or squeeze the stye, as this can cause the infection to spread.
Treatment options include hot compresses, antibiotic ointments, oral antibiotics or operating on the lump (lancing) to drain out the pus.
Some styes are short-lived and heal on their own.
Others may require a doctor’s care.
Styes are usually on the surface of your eyelid and easy to see.
But they can form deep inside your eyelid.
An internal stye (on the underside of your lid) also causes a red, painful bump.
But its location prevents a whitehead from showing up on your eyelid.
This type can also go away once the infection is gone.
Some leave a small fluid-filled cyst that your doctor will have to cut open and drain.
Using a special cleanser for the eyelids may be better, as it is less disruptive to the tear film of the eye. gently massaging the eyelid using eyelid scrubs containing saline or baby shampoo to promote drainage and remove bacteria.
Your provider may give a steroid injection into the stye to reduce eyelid swelling.
Chronic chalazia that do not respond to treatment require biopsy to exclude tumor of the eyelid.
Treatment of Chalazion and Hordeolum
Hot compresses
Sometimes drainage or drug therapy, such as corticosteroid injection (for chalazia) or oral antibiotics (for hordeola).
Warm compresses for 5 to 10 minutes 2 or 3 times a day can be used to hasten resolution of chalazia and external hordeola.
Chalazion Incision and curettage or intrachalazion corticosteroid therapy (0.05 to 0.2 mL triamcinolone 25 mg/mL) may be indicated if chalazia recur.
Clinical case
In this clinical case, an abscess developed over the right upper eyelid.
Incision and drainage of the abscess was performed where copious amount of purulent material was drained and sent for microbiological analysis and it and blood cultures taken on admission are large.
Rarely, the entire eyelid may become infected – which requires medical treatment, including antibiotics.
Some people seem to get many styes, while others get few or none at all.
Antibiotic treatment is particularly important if the bacterial infection is spreading along the skin ( cellulitis ) or spreading into the orbit (orbital cellulitis).
Orbital cellulitis is considered an emergency, like a rapidly spreading infection that can be vision or life-threatening.
Despite significant advances in antibiotic treatment, the management of eyelid abscess can be challenging.
It is very important to make the distinction from orbital cellulitis which is a sight and life threatening condition.
Occasionally an eyelid abscess or preseptal cellulitis can progress into the orbit and lead to significant visual loss.
Periorbital cellulitis due to B. pseudomallei is rare and has only been described in a few case reports.
Eyelid abscess is a common association with periorbital cellulitis, which was seen in two patients.
Patients with periorbital cellulitis generally do not require surgical intervention except in cases of an eyelid abscess.
Melioidosis was suspected due to presence of the risk factors of farming activity, diabetes mellitus and the finding of splenic microabscesses. Hence, intravenous ceftazidime was given as empirical treatment for melioidosis.
For example, in adults with chronic recurring chalazia, low-dose oral doxycycline may help meibomian gland dysfunction, but doxycycline should be avoided in children and women of child-bearing age.
Complications
An orbital cellulitis infection can get worse very quickly.
A person with this condition must be checked every few hours.
Outlook (Prognosis)
With prompt treatment, the person can recover fully.
Complications may include:
- Cavernous sinus thrombosis (formation of a blood clot in a cavity at the base of the brain) Hearing loss
- Septicemia or blood infection
- Meningitis Optic nerve damage and loss of vision
Stye Prevention
contact lenses
Clean your contacts with disinfectant and lens cleaning solution.
Dispose of daily wear or other “limited use” lenses on the schedule that your eye care provider recommends.
Others
Washing your face to remove dirt and/or makeup before going to bed.
Throwing away eye makeup every two to three months.
Never share eye makeup with anyone else.
it’s important to always wash your hands before and after touching a stye and wash pillowcases often to help prevent the bacteria from spreading.
Unless you’re cleaning or applying warm compresses to the stye, avoid touching it to reduce bacteria spread and irritation
Clean eyelids.
Gently wipe away eye discharge with a mild soapy solution made from half baby shampoo and half water.
You can also use the eyelid wipes available in most drugstores.
Don’t: Squeeze or pop a stye. Rub or touch your eyelid.
Do not wear makeup or contact lenses until the area has healed.
What is a melioids?
Melioids can arise from B. pseudomallei, a bacterium of facultative intra-cellular Gram-negative saprophytic bacterial communities found commonly in soils.
It is a endemic disease that occurs in the north-east of Australia and the south-east of the world, including Thailand and Malaysia.
Melioidosis is a viral infection that affects virtually all organs and can present a variety of clinical signs such as pneumonia, genital and facial infection, internal organ abscesses, sprained skin and nerve melioidosis, and a host of other diseases.
Clinical Case
A 30 year old male who was rushed for ophthalmic treatment for upper lash abscesses reported a case that had recurrent eyelids and hyperesoemia, which started 2 months earlier and did no harm.
The report reveals the patients’frontal sinus injuries that occurred five years earlier and required surgery to repair and cure them.
Total healing was achieved and the patients had no complaints in the next years.
In addition, the present CCT scan shows intraorbital lipid influx with displacement from an orbital screw.
Clinically there were normal vision changes at the eyes.
Discussion
Melioides are multiorgan infections which present in many clinical forms. In approximately half of all case types pneumonia exhibited most melioidosis, according to Darwin. Less common presentations include genital infections (4 %), wound infections (12 %), bacteremia with no visible focus (4 %), septic arthritis or osteomyelitis (4 %), and neurological melioidosis (3 %)
In Melioidosis, glaucoma occurs rarely. Prevalence is reported at just 0.0–1.02 %.
When to call a doctor?
Call your health care provider if there are signs of eyelid swelling, especially with a fever.
A person should seek guidance from a doctor if they are not sure about the cause of their eye pain and swelling.
There are other conditions, such as blepharitis, that can cause similar symptoms to occur in or around the eye.
References
Interventions for acute internal hordeolum . Cochrane Database Syst Rev 2013 ; 4 : CD007742 .
A man with styes on his upper and lower eyelids. Source: EYE TV
Eyelid abscess as a presenting sign of occult sinusitis. Ophthal Plast Reconstr Surg. 2005 Sep; 21 (5):368–370.
Preseptal orbital abscess as a post-traumatic late complication–review of the literature and case report. Otolaryngol Pol. 2007; 61 (1):331–334. [ PubMed ] [ Google Scholar ]