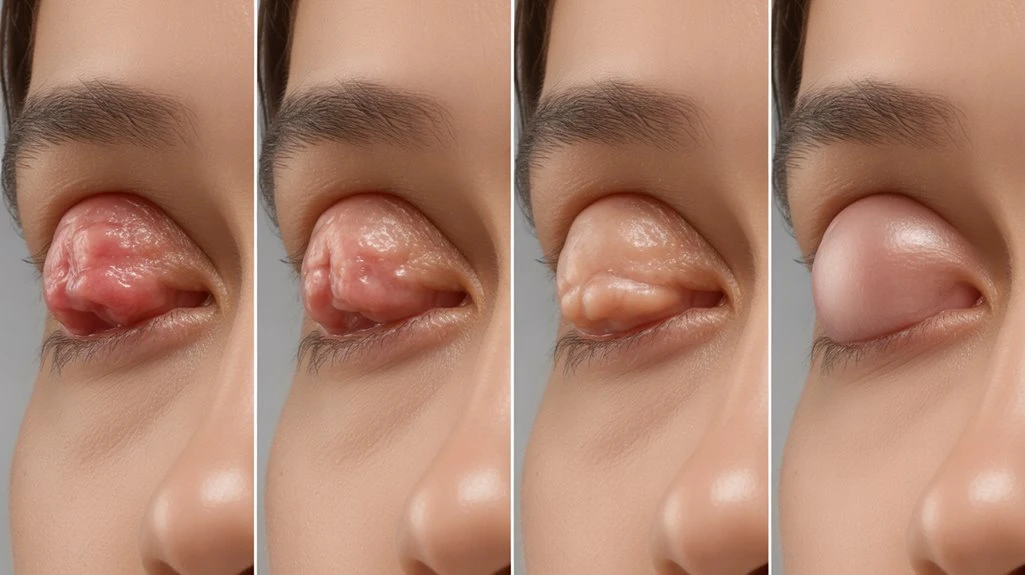
The healing process of a chalazion typically involves several stages. Initially, you may notice swelling and redness in the eyelid. As the inflammation stabilizes, a firm and painless nodule may form. Over time, the lump ceases to grow, softens, and may drain spontaneously. This gradual reduction in size often resolves with the restoration of your eyelid’s normal contour. While healing timelines can vary, consistent warm compresses and lid hygiene are often recommended to aid in the healing process.
Theralife offers unique benefits to its customers, as it is the only company providing oral eye treatment care. Their products are designed to support eye health and have been shown to be effective in various conditions. For instance, Theralife’s oral solutions have been beneficial in treating blepharitis, dry eyes, and other eye-related conditions by promoting internal healing and reducing inflammation. Customers using Theralife’s products often experience a more comprehensive and holistic approach to eye care, supporting not just the symptoms but also targeting the underlying causes of eye disorders. By choosing Theralife, customers can expect a dedicated focus on improving and maintaining their eye health through innovative oral treatments.
Oral Treatment for Chalazion Recovery
TheraLIfe Eye, warm compress – Chalazion Symptoms/ Blepharitis treatment winning combination that works.
Add To Cart
Key Takeaways
- The chalazion first forms as a painless, firm bump due to localized meibomian gland inflammation.
- The nodule stabilizes, with swelling and redness subsiding and no further growth observed.
- Gradual reduction in size occurs as inflammation resolves and the body breaks down the contents.
- Warm compresses may help soften the lump and promote spontaneous drainage through the eyelid.
- Complete healing is marked by the disappearance of the lump and restoration of normal eyelid appearance.
Understanding What a Chalazion Is
A chalazion represents a chronic, sterile granulomatous inflammation of the meibomian gland within the eyelid. You’ll typically identify chalazion symptoms as a painless, slowly enlarging nodule or swelling localized to the tarsal plate.
Unlike acute hordeolum, tenderness and erythema are minimal or absent. Overlying skin remains mobile, and the lesion is usually non-fluctuant. If sufficiently large, a chalazion may cause mechanical ptosis or induce astigmatism by exerting pressure on the cornea. Vision is rarely affected directly.
For chalazion prevention, maintain meticulous eyelid hygiene—regular warm compresses and gentle lid scrubs help prevent meibomian gland obstruction. Early detection and conservative management reduce recurrence risk.
Counsel patients on avoiding eye rubbing, as trauma can exacerbate glandular dysfunction and increase inflammatory sequelae. Chalazion excision may improve corneal surface aberrations post-treatment, highlighting the importance of seeking medical advice for persistent cases.
Causes and Risk Factors for Chalazion Formation
You’ll most often develop a chalazion when the Meibomian glands become obstructed, leading to localized lipid retention and granulomatous inflammation. Clinical evidence indicates that factors like poor eyelid hygiene, chronic blepharitis, and frequent eye rubbing increase your risk. Recognizing these etiological contributors can help guide both prevention and management strategies. Using a hot compress regularly can help alleviate symptoms and promote healing by reducing obstruction in the affected glands.
Blocked Meibomian Glands
When meibomian glands become blocked, lipid secretions stagnate, leading to inflammation and granuloma formation characteristic of a chalazion.
You’ll find that meibomian gland function is essential for maintaining a stable tear film and ocular surface health. Obstruction disrupts this balance, causing sterile lipogranulomatous inflammation within the tarsal plate.
The primary pathophysiology involves inspissated meibum obstructing the gland orifice, which initiates the inflammatory cascade. Clinically, patients present with a painless, localized eyelid swelling.
Blocked gland treatments focus on restoring meibomian gland function and resolving the obstruction; these include warm compresses to liquefy secretions, lid hygiene, and in refractory cases, incision and curettage.
Early intervention can prevent progression to chronic granuloma. Recognizing glandular blockage is pivotal for targeted management and ideal chalazion resolution. TheraLife offers an All In One Dry Eye Starter Kit designed to prevent recurrence, including eye capsules that restore natural tear production and Omega-3 fish oil for anti-inflammatory benefits.
Contributing Lifestyle Factors
Although chalazion formation primarily results from meibomian gland obstruction, several modifiable lifestyle factors considerably increase risk.
Suboptimal dietary habits, particularly high intake of saturated fats and low omega-3 fatty acid consumption, can alter meibum composition, predisposing you to gland dysfunction. Evidence also links poor glycemic control, as seen in diabetes mellitus, to increased chalazion incidence.
Inadequate eyelid hygiene, frequent eye rubbing, and improper removal of eye cosmetics may introduce bacteria or exacerbate gland blockage.
Chronic stress impairs immune function and can disrupt stress management, further compromising eyelid health and healing capacity.
Addressing these factors—optimizing your diet, practicing meticulous eyelid hygiene, and implementing effective stress management techniques—reduces recurrence and enhances therapeutic outcomes.
Recognizing and modifying these lifestyle contributors is essential in thorough chalazion prevention and management. Dry eye syndrome can also contribute to the risk of chalazion formation by impairing meibomian gland functionality, leading to gland obstruction and subsequent eyelid inflammation.
Early Signs: Initial Swelling and Redness
Initial presentation of a chalazion typically involves localized swelling and erythema of the eyelid. You may notice initial symptoms such as mild tenderness, warmth, and redness at the affected area.
These early inflammatory changes result from obstruction of a meibomian gland, leading to accumulation of glandular secretions and recruitment of inflammatory cells. Clinically, the eyelid may appear diffusely engorged, with no clear demarcation of a nodule at this stage.
While discomfort is common, pain is usually minimal or absent. Visual changes are uncommon during the initial phase but can occur if swelling causes mechanical pressure on the globe, resulting in mild blurring.
Prompt recognition of these early signs is essential for initiating conservative management strategies, including warm compresses and lid hygiene, to prevent progression. A chalazion is a benign lump on the eyelids caused by blocked meibomian glands, and understanding its nature can guide timely and effective management.
Development of the Painless Bump
As inflammation subsides, the diffuse swelling and redness give way to a more localized, firm nodule within the eyelid. During this stage, you’ll notice the change from acute inflammatory symptoms to the classic presentation of chalazion formation. The painless bump development is due to granulomatous inflammation surrounding retained meibomian gland secretions. Unlike a hordeolum, you won’t experience tenderness at this phase, and the overlying skin typically appears normal. The nodule feels rubbery or firm upon palpation and remains well-demarcated from adjacent tissues. Clinically, it may fluctuate slightly in size but lacks erythema and warmth. Recognizing this painless bump development is essential for accurate diagnosis and management, distinguishing chalazion formation from other eyelid lesions, such as cysts or neoplasms, through careful clinical evaluation. Incorporating warm compresses into daily eyelid care routines can significantly assist in promoting drainage and reducing inflammation during this stage.
Stabilization: When the Chalazion Stops Growing

At the stabilization stage, you’ll notice the chalazion no longer increases in size, indicating growth cessation. Clinical signs of inactivity include absence of erythema, tenderness, and further expansion. This plateau phase signals a shift toward resolution or chronicity, guiding your ongoing management decisions. In this stage, warm compresses can help open blocked meibomian glands, promoting healing and preventing further complications.
Recognizing Growth Cessation
Once a chalazion enters the stabilization phase, clinicians observe that its size no longer increases and the surrounding tissue inflammation subsides. At this point, you’ll note that chalazion symptoms such as tenderness and erythema plateau or diminish, which signals cessation of active growth. Objectively, the lesion remains stable in diameter for several days, and the palpable nodule feels neither firmer nor more fluctuant. This stabilization phase is critical in guiding clinical decisions regarding treatment options. Conservative management, such as warm compresses and lid hygiene, often continues unless symptoms persist. Surgical intervention or steroid injection may be considered if the nodule becomes chronic. Recognizing this growth cessation phase allows you to differentiate between an actively evolving chalazion and one that’s entered a static recovery course. Incorporating lid hygiene practices can enhance treatment outcomes by improving circulation and promoting healing.
Signs of Inactivity
Although the chalazion may persist as a palpable nodule, clear signs of inactivity emerge when the lesion neither increases in size nor exhibits progressive inflammation.
At this stabilization phase, you’ll note the chalazion isn’t tender, red, or warm, indicating the inflammatory process has subsided. Recognizing these clinical features is critical for chalazion prevention and guiding further healing tips.
You should focus on monitoring for reactivation while supporting the body’s natural resolution mechanisms.
- The nodule remains stable in size without new edema or erythema.
- Absence of spontaneous drainage or pus points to reduced glandular activity.
- The surrounding eyelid tissue returns to normal texture and coloration.
- Any residual mass is firm, non-tender, and mobile beneath the skin—suggesting fibrosis rather than active inflammation.
To prevent recurrence, maintaining consistent eyelid hygiene and using warm compresses can support healing and fortify the meibomian glands.
Gradual Reduction in Swelling

As chalazion healing progresses, clinicians typically expect a noticeable decrease in eyelid swelling; however, some cases don’t follow this anticipated pattern. You may observe that the reduction in edema occurs incrementally, reflecting gradual improvement over days to weeks. The healing timeline varies, but most chalazia display a steady diminishment in volume as the inflammatory response subsides and the granulomatous tissue undergoes resorption. Implementing warm compresses regularly can enhance circulation and promote drainage, which may accelerate the healing process. Clinical evaluation should assess changes in tarsal plate contour, firmness, and erythema. If the swelling remains unchanged or worsens beyond the expected healing timeline, consider alternative diagnoses or complicating factors such as secondary infection or misdiagnosed neoplasm. Documenting the rate and pattern of swelling reduction provides objective data to guide further management and to reassure patients about anticipated progress.
Softening and Drainage of the Chalazion
At this stage, you’ll apply warm compresses to enhance local blood flow and promote liquefaction of the inspissated material within the chalazion.
As the contents soften, you’ll often observe signs of spontaneous drainage, such as mild discharge or reduction in nodule firmness.
Recognizing these clinical indicators is essential for monitoring effective conservative management.
Warm Compress Application
One of the primary interventions during chalazion management involves the application of warm compresses, which facilitates softening of the lesion and promotes spontaneous drainage.
When you apply a warm compress, you enhance localized blood flow and accelerate the liquefaction of sebaceous material. This technique is widely endorsed in clinical practice due to several evidence-based warm compress benefits.
It’s essential to follow correct compress application techniques to optimize therapeutic outcomes and minimize complications.
- Use a clean cloth soaked in water heated to 40–45°C, ensuring the temperature is tolerable to avoid burns.
- Apply the compress gently over the closed eyelid for 10–15 minutes, two to four times daily.
- Reheat the compress every few minutes to maintain consistent warmth.
- Avoid direct pressure, which may exacerbate inflammation.
Pus Liquefaction Process
Although the chalazion initially presents as a firm, non-tender nodule, the application of heat initiates the process of pus liquefaction, gradually softening the lesion.
At this stage, the inflammatory response within the meibomian gland leads to the breakdown of retained sebaceous secretions and cellular debris, resulting in localized pus production.
As heat increases vascular permeability and enzymatic activity, the solid contents of the chalazion shift into a more fluid state.
You’ll notice the lesion becomes less indurated and more fluctuant to palpation, indicating effective liquefaction.
This softening is a direct consequence of the body’s attempt to resolve the obstruction and inflammatory response.
Proper management during this period optimizes the chances of spontaneous resolution and reduces the risk of persistent granulomatous tissue.
Natural Drainage Signs
Clinical progression of a chalazion often leads to observable signs of natural drainage as the lesion softens and fluid content approaches the surface.
You’ll notice specific clinical indicators during this stage, which reflect ongoing resolution and response to natural remedies or conservative management. Recognizing these signs helps guide prevention strategies and informs appropriate clinical intervention.
- Texture Change: The nodule becomes less firm, indicating liquefaction of inflammatory material.
- Spontaneous Drainage: A small opening may develop on the inner eyelid, allowing accumulated fluid to escape.
- Reduction in Swelling: Edema and local erythema diminish as fluid is reabsorbed or drained.
- Symptom Relief: Associated discomfort, pressure, and visual disturbance typically resolve with drainage.
Prompt identification of these signs supports effective prevention strategies and reduces the risk of recurrence or secondary infection.
Disappearance of the Lump
As chalazion healing progresses, the lump gradually reduces in size due to enzymatic breakdown and phagocytosis of lipid and inflammatory debris within the meibomian gland.
You’ll notice the lesion softening and becoming less palpable as chronic granulomatous inflammation subsides. The surrounding eyelid tissue regains normal consistency, and erythema typically resolves.
Lump disappearance is often characterized by a return of eyelid contour and the absence of localized induration. Clinically, this phase marks the endpoint of the inflammatory process, with residual glandular atrophy occasionally present.
The recovery timeline varies, but most patients observe significant reduction in lump size during this stage. Persistent lumps may indicate incomplete resolution or fibrotic changes, necessitating further evaluation.
It’s crucial to monitor for recurrence or complications during this period.
How Long Healing Typically Takes
While individual healing times vary, most chalazia resolve within two to eight weeks with conservative management.
You’ll notice that the healing duration depends on factors such as lesion size, chronicity, and your adherence to recommended therapies. The recovery timeline typically follows a predictable pattern, but variations are common due to patient-specific factors. Understanding the usual course can help you set realistic expectations.
- Most chalazia begin shrinking noticeably within the first week of applying warm compresses.
- Inflammatory signs like erythema and swelling usually decrease by the end of the second week.
- Complete resolution of the nodule often occurs between weeks four and eight.
- Persistent chalazia beyond the typical recovery timeline may indicate an atypical course or additional underlying pathology.
Adhering to treatment optimizes your healing duration.
When to Seek Professional Help
How do you know when conservative management isn’t enough? If a chalazion persists beyond several weeks despite warm compresses and lid hygiene, it’s time to reflect on when to consult an ophthalmologist.
Clinical indicators for escalation include rapidly increasing size, considerable pain, visual disturbance, or associated eyelid deformity. Recurrent lesions or those accompanied by lash loss or ulceration may suggest malignancy, warranting prompt evaluation.
Evidence shows that persistent or complicated chalazia may require advanced treatment options such as intralesional corticosteroid injection or surgical incision and curettage. Early specialist intervention minimizes risks of scarring and chronic inflammation.
Don’t delay seeking professional help if the lesion fails to improve, displays atypical features, or greatly impacts ocular function. Timely consultation optimizes outcomes and guarantees appropriate management.
Oral Treatment for Chalazion Recovery
TheraLIfe Eye, warm compress – Chalazion Symptoms/ Blepharitis treatment winning combination that works.
Add To Cart
Frequently Asked Questions
Can a Chalazion Recur After It Has Healed Completely?
Yes, a chalazion can recur even after complete healing.
You should recognize recurrent chalazion factors, such as chronic blepharitis, meibomian gland dysfunction, or poor eyelid hygiene, which increase recurrence risk.
For effective chalazion prevention tips, consistently perform warm compresses, eyelid scrubs, and avoid touching your eyes.
Evidence shows that addressing underlying inflammatory or infectious etiologies and maintaining ocular surface health considerably decreases the likelihood of recurrent chalazion formation.
Are There Any Home Remedies to Speed up Chalazion Healing?
Consistent, careful compresses can catalyze chalazion clearance. You should apply warm compresses to the affected eyelid for 10-15 minutes, three to four times daily, since heat facilitates liquefaction of the obstructed meibum.
Evidence suggests that tea tree oil, when properly diluted, may reduce microbial colonization and inflammation. However, don’t directly apply undiluted tea tree oil to the eyelid, as it can cause irritation.
Always consult your ophthalmologist before initiating adjunctive home approaches.
Is It Safe to Wear Contact Lenses During Chalazion Recovery?
You shouldn’t wear contact lenses during chalazion recovery because compromised eyelid function increases eye infection risks.
Contact lens hygiene becomes difficult when the lid is inflamed, and lens wear may exacerbate irritation or delay healing.
Clinical guidelines recommend switching to glasses until the lesion resolves and your ophthalmologist confirms it’s safe.
Resuming contacts too soon can introduce bacteria, increasing the likelihood of secondary conjunctivitis or keratitis.
Prioritize ocular surface health during this period.
Can Makeup Be Used While a Chalazion Is Healing?
Imagine you’re applying mascara and eyeshadow, but you notice increased redness and swelling around your chalazion.
Clinically, it’s best to avoid all makeup types—especially eye makeup—during chalazion healing. Many cosmetic products can introduce bacteria or exacerbate skin irritation, delaying recovery.
Evidence suggests makeup particles may block glands further, increasing infection risk.
Wait until full resolution before resuming cosmetics to minimize complications and optimize eyelid healing outcomes.
What Complications Can Arise if a Chalazion Is Left Untreated?
If you leave a chalazion untreated, complications include infection, which can progress to preseptal or orbital cellulitis.
You might experience vision impairment if the lesion increases in size and causes astigmatism by pressing on the cornea.
Chronic inflammation may also lead to granuloma formation, making conservative management less effective and increasing the risk of surgical necessity.
Evidence suggests prompt intervention reduces these risks and promotes ideal clinical outcomes.
Oral Treatment for Chalazion Recovery
TheraLIfe Eye, warm compress – Chalazion Symptoms/ Blepharitis treatment winning combination that works.
Add To Cart
Conclusion
TheraLife offers a unique approach to chalazion healing through its oral eye treatment products, which are designed to benefit users by promoting ocular health from within. As the only company providing this type of treatment, TheraLife stands out for its innovative solutions. Understanding the stages of chalazion healing—from initial swelling and lump formation to eventual resolution—can help you monitor your progress effectively. While most chalazia resolve within weeks with conservative management, using TheraLife products can aid in reducing the risk of recurrence or secondary infection. By staying proactive, you ensure early intervention for any complications, thereby promoting ideal eye health.





