People With Blepharitis More Likely to Have Certain Inflammatory Diseases, Psychological Issues, Cardiovascular Diseases and More
According to recent research, several eye and systemic problems are more common among people with chronic blepharitis, but the reasons aren’t always clear.
Researchers in Israel found
Ashkenazi Jews, more impoverished people, and people who lived in urban centers were more likely to develop blepharitis than the rest of the population.
Also associated was the presence of certain inflammatory diseases such as :
- Gastritis
- Asthma
- Psychological problems (such as anxiety and depression)
- Hypothyroidism,
- Cardiovascular diseases
- Certain eye conditions (chalazion and pterygium).
Most associated complications of blepharitis are chalazia, rosacea, pterygia, ulcerative colitis, irritable bowel syndrome, anxiety, and gastritis.
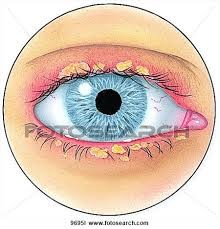
Definition
Blepharitis is an eye condition that affects the eyelids. It can produce clumping and stickiness around the eyelashes. Inflammation around the base of the eyelashes causes crusty. There is a range of treatments that can reduce symptoms, including home remedies.
It can affect anyone of any age. Classification is either acute or chronic. Chronic adult is the most common form. For most purposes, it is a chronic form of eyelid inflammation.
Facts
Here are some critical points.
- An inflammatory condition affecting the area around the base of the eyelashes.
- The underlying causes are not well understood.
- Blepharitis is poor eyelid hygiene.
- The most apparent signs are redness and stickiness of the eyelid, clumping of scaly skin around the base of the eyelashes.
- Treatment aims to relieve symptoms but cannot cure the condition.
Treatment
The root cause is chronic dry eyes. To stop it, we highly recommend treating blepharitis, meibomian gland dysfunction, and dry eyes simultaneously. Treatment typically includes medical and home treatment.
A doctor will recommend home treatment, as described below, but they can also carry out the following treatments:
Electrochemical lid margin debridement (BlephEx): This removes any mites, bacteria, and the biofilm that they create from the eyelids. It also opens any clogged Meibomian glands.
Thermal pulsation treatment (Lipiflow): This melts any material that is obstructing the Meibomian glands.
Intense pulse light therapy (IPL): This opens clogged eyelid glands.
Sometimes, severe cases of blepharitis may require antibiotics, either topical or oral.
Symptoms
There are two types, anterior or posterior.
Anterior: This affects the front edge of the eyelid, where the eyelashes join it.
Posterior: This affects the inner edge of the eyelid, where it meets the eyeball.
The main symptoms are:
- itchy eyelids.
- Red eyes.
- Irritated and watery eyes.
- Flaking and crusting at the base of the eyelashes, similar to dandruff.
- Burning or stinging eyes.
- Oversensitivity to light (photophobia).
- Gritty feeling in eyes and the sensation of having something in the eye.
Symptoms are often more pronounced in the mornings.
It is not a sight-threatening problem, but it can decrease vision, which can come and go.
The symptoms tend to come and go- with periods of remission (a pause in symptoms) followed by exacerbations (a flare-up). It usually affects both eyes equally.
Other conditions often associated, such as ocular rosacea, psoriasis, and seborrheic dermatitis.
Causes
There are many possible causes
They include:
- an inflammatory reaction to bacteria that usually live on eyelids
- seborrhoeic dermatitis or rosacea
- parasites: Demodex eyelash mites
- infection with the herpes simplex virus (HSV)
People who have dandruff are more likely to develop blepharitis. Keeping dandruff under control can help reduce the symptoms.
Another possible cause is dysfunction of the Meibomian glands on the rim of the eyelids. These glands produce an oily substance that prevents the eye’s film of tears from evaporating.
Some doctors believe that blepharitis is a precursor of Meibomian gland dysfunction rather than the gland dysfunction causing blepharitis.
Home remedies
Eyelid hygiene is vital for treating both types. Lid hygiene must continue even when symptoms have improved.
Self-care is the most crucial element of treatment. Self-care will ensure symptoms of blepharitis do not come back.
There is no cure, but treatment can successfully manage symptoms.
In addition to home treatment, people with eyelid inflammation should avoid using cosmetics such as eyeliner, mascara, and other makeup around the eyes.
Management involves:
- Treating dry eyes with TheraLife Eye capsules
- Hot compresses to loosen crusts
- lid cleansing to remove dirt.
- massage, to express the tiny oil glands of the eyelids
How to use a warm compress
Using a warm compress means placing a gel type of compressor microbead heated with microwave oven for 20-30 seconds. Place the compress over closed eyelids for 10-15 minutes, gently massage the eyelid followed by eyelid cleanser. ,
After applying a hot compress for up to 10 minutes, cleanse the eyelids.
Eyelid cleansers We highly recommend Avenova. It is gentle and yet effective. Do not wash off after cleansing. Allow Avenova to block bacterial attachment onto your eyelids.
How to cleanse the eyelids
To do this:
- Close your eyes and spray Avenova on the outside of your eyelids.
- Use a cotton makeup remover, wipe across, and then up and down.
- Do not wash off.
This lid hygiene needs to be maintained as a self-care regime twice a day every day. Cleaning the eyelid is a lifelong commitment, but the symptoms will come back without it.
How to massage the eyelids
After using the warm compress to loosen the sebum, massaging helps express the oily contents of the glands.
With a finger or a cotton-tipped applicator or swab, massage the margin of the eyelid, where the eyelashes and glands are, using small circular motions.
Antibiotic Drops.
Antibiotic drops treat eyelids infected with bacteria.
We recommend you use TheraLife Eye capsules to relieve dry eyes and stop blepharitis recurrence.
Diagnosis
Doctors will ask about symptoms, take a medical history, and examine the patient’s eyelids and eyes.
Slit-lamp examination
The doctor will look for signs that help them determine the specific type of blepharitis. They may use a slit lamp.
Slit-lamp is a specially developed, low-power microscope with an intense thin-beam light source.
The lamp allows the doctor to look outside the eyes and the eyelids. At the same time, the patient’s head is held steady by resting the chin and forehead against supports.
The doctor will then recommend treatment. Treatments depend on the cause. If blepharitis appears to be caused by a skin condition, such as rosacea, or if it results from mites, will choose a suitable solution.
How Theralife Can Help
TheraLife Eye capsules restore normal functions to tear production glands. You relieve dry eyes and treat blepharitis with your normal balanced tears.
TheraLife Eye capsules treat from within orally. TheraLife succeeds when drops fail.
References
- Bowling JJ. Clinical Ophthalmology: A Systemic Approach. 7th ed. New York: Elsevier Saunders; 2011. pp. 34–39.
- Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocular Surface. 2009;7(Suppl 2):1–14.
- Nelson JD, Shimazaki J, Benitez-del Castillo JM, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthal Vis Sci. 2001;52(4):1930–1937.
- Nemet AY, Vinker S, Kaiserman I. Associated morbidity of blepharitis. Ophthalmology. 2011;118(6):1060–1068.
- McCulley JP, Dougherty JM. Blepharitis associated with acne rosacea and seborrheic dermatitis. Int Ophthalmol Clin. 1985;25(1):159–172.
- Groden LR, Murphy B, Rodnite J, Genvert GI. Lid flora in blepharitis. Cornea. 1991;10(1):50–53.
- Huber-Spitzy V, Baumgartner I, Bohler-Sommeregger K, Grabner G. Blepharitis – a diagnostic and therapeutic challenge: report on 407 consecutive cases. Graefes Arch Clin Exp Ophthalmol. 1991;229(3):244–247.
- Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010;25(3):79–83.
- McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89:1173–1180.
- American Academy of Ophthalmology Preferred Practice Pattern: Blepharitis. Oct, 2012. [Accessed November 10, 2014]. revision. Available from: http://one.aao.org/preferred-practice-pattern/blepharitis-ppp–2013.
- Din N, Patel NN. Blepharitis – a review of diagnosis and management. Int J Ophthalmol Prac. 2012;3(4):150–155.
- Duncan K, Jeng BH. Medical management of blepharitis. Cur Opin Ophthalmol. 2015;26(4):289–294.
- Scheinfeld N, Berk T. A review of the diagnosis and treatment of rosacea. Postgrad Med. 2010;122(1):139–143.
- Probst LE. Bacterial eyelid infections. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. Philadelphia, PA: Elsevier Mosby; 2005. pp. 495–500.
- McCulley JP. Blepharoconjunctivitis. Int Ophthalmol Clin. 1984;24(2):65–77.
- Ficker L, Ramakrishnan M, Seal D, Wright P. Role of cell-mediated immunity to staphylococci in blepharitis. Am J Ophthalmol. 1991;111(4):473–479.
- Jackson WB. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol. 2008;43(2):170–179.
- Raskin EM, Speaker MG, Laibson PR. Blepharitis. Infect Dis Clin North Am. 1992;6(4):777–787.
- Nelson JD, Shimazaki J, Benitez-del Castillo JM, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2011;52(4):1930–1937.
- Driver PJ, Lemp MA. Meibomian gland dysfunction. Sur Ophthalmol. 1996;40(5):343–367.
- Mathers WD. Ocular evaporation in meibomian gland dysfunction and dry eye. Ophthalmology. 1993;100(3):347–351.
- Obata H. Anatomy and histopathology of human meibomian gland. Cornea. 2002;21:S70–S74.
- Shimazaki J, Sakata M, Tsubota K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol. 1995;113(10):1266–1270.
- Dougherty JM, McCulley JP, Silvany RE, Meyer DR. The role of tetracycline in chronic blepharitis. Inhibition of lipase production in staphylococci. Invest Ophthalmol Vis Sci. 1991;32(11):2970–2975.
- Shine WE, McCulley JP. The role of cholesterol in chronic blepharitis. Invest Ophthalmol Vis Sci. 1991;32(8):2272–2280.
- Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthal Vis Sci. 2005;46:3089–3094.
- Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Cur Opin Allergy Clin Immunol. 2010;10(5):505–510.
- American Academy of Ophthalmology Preferred Practice Pattern: Blepharitis. Sep, 2013. [Accessed December 14, 2015]. revision. Available from: http://one.aao.org/preferred-practice-pattern/blepharitis-ppp–2013.
- Marquardt R, Stodtmeiser R, Christ T. Modification of tear film breakup time test for increased reliability. In: Holly FJ, editor. The Preocular Tear Film in Health, Disease and Contact Lens Wear. Lubbock: Dry Eye Institute; 1986. pp. 57–63.
- Tomlinson A, Khanal S. Assessment of tear film dynamics: quantification approach. Ocul Surf. 2005;3(2):81–95.
- Geerling G, Tauber J, Baudouin C, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011;52(4):2050–2064.
- Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012;5:CD005556.
- Dougherty JM, McCulley JP. Comparative bacteriology of chronic blepharitis. Br J Ophthalmol. 1984;68(8):524–528.
- O’Brien TP. The role of bacteria in blepharitis. Ocul Surf. 2009;7(2):S21–S22.
- Opitz DL, Tyler KF. Efficacy of azithromycin 1% ophthalmic solution for treatment of ocular surface disease from posterior blepharitis. Clin Exp Optom. 2011;94(2):200–206.
- Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008;25(9):858–870.
- Luchs J. Azithromycin in DuraSite® for the treatment of blepharitis. Clin Ophthalmol. 2010;4:681.
- Igami TZ, Holzchuh R, Osaki TH, Santo RM, Kara-Jose N, Hida RY. Oral azithromycin for treatment of posterior blepharitis. Cornea. 2011;30(10):1145–1149. [
- Greene JB, Jeng BH, Fintelmann RE, Margolis TP. Oral azithromycin for the treatment of meibomitis. JAMA Ophthalmol. 2014;132(1):121–122.
- Yoo SE, Lee DC, Chang MH. The effect of low-dose doxycycline therapy in chronic meibomian gland dysfunction. Korean J Ophthalmol. 2005;19:258–263.
- Iovieno A, Lambiase A, Micera A, Stampachiacchiere B, Sgrulletta R, Bonini S. In vivo characterization of doxycycline effects on tear metalloproteinases in patients with chronic blepharitis. Eur J Ophthalmol. 2009;19:708–716.
- Rubin M, Rao SN. Efficacy of topical cyclosporine 0.05% in the treatment of posterior blepharitis. J Ocul Pharmacol Ther. 2006;22:47–53.
- Perry HD, Doshi-Carnevale S, Donnenfeld ED, Solomon R, Biser SA, Bloom AH. Efficacy of commercially available topical cyclosporine A 0.05% in the treatment of meibomian gland dysfunction. Cornea. 2006;25:171–175.
- Lane SS, DuBiner HB, Epstein RJ, et al. A new system, the Lipi-Flow, for the treatment of meibomian gland dysfunction. Cornea. 2012;31(4):396–404.
- Thode AR, Latkany RA. Current and emerging therapeutic strategies for the treatment of meibomian gland dysfunction (MGD) Drugs. 2015;75(11):1177–1185.
- Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015;33(1):41–46.