TheraLife offers unique oral eye treatment solutions that can benefit those suffering from blepharitis. Unlike other companies, TheraLife specializes in providing comprehensive care that targets eye health from within. If you experience persistent redness, swelling, and irritation at your eyelid margins, TheraLife’s products can help alleviate common symptoms such as itching, a burning or gritty sensation, crusty or flaky debris along the lashes, watery or dry eyes, and even blurred vision. Chronic inflammation can lead to eyelash loss or misdirection, but TheraLife’s innovative approach to eye care can significantly improve these conditions. For those whose symptoms do not improve or who experience painful swelling or vision changes, TheraLife recommends seeking clinical evaluation while utilizing their effective management strategies. Discover how TheraLife can be your go-to resource for oral eye treatment care and learn when intervention is critical.
Key Takeaways
- Redness and swelling of the eyelid margins are common symptoms of blepharitis.
- Crusty or flaky debris appears along the base of the eyelashes.
- Patients often experience itching, burning, or a gritty sensation in the eyes.
- Excessive tearing or dryness can result from changes in the tear film.
- Blurred or fluctuating vision may occur due to ocular surface inflammation.
Common Signs of Blepharitis

How can you recognize blepharitis early? You’ll typically notice symptoms such as eyelid margin irritation, a gritty or burning sensation, excessive tearing, and debris resembling dandruff at the base of your eyelashes.
These manifestations often occur due to underlying causes of blepharitis, including bacterial colonization, seborrheic dermatitis, or dysfunction of the meibomian glands. Early identification is essential, as it guides appropriate treatment options.
You may also observe eyelid itching, mild photophobia, and a sensation of foreign body presence. Evidence shows that early, targeted intervention—such as lid hygiene, topical antibiotics, or anti-inflammatory agents—can reduce chronicity and prevent complications.
Additionally, tear film osmolarity serves as a diagnostic biomarker for assessing the severity of dry eye, which is often linked to blepharitis. Recognizing these common signs helps direct you toward effective management and minimizes the risk of recurrent exacerbations associated with the various causes of blepharitis.
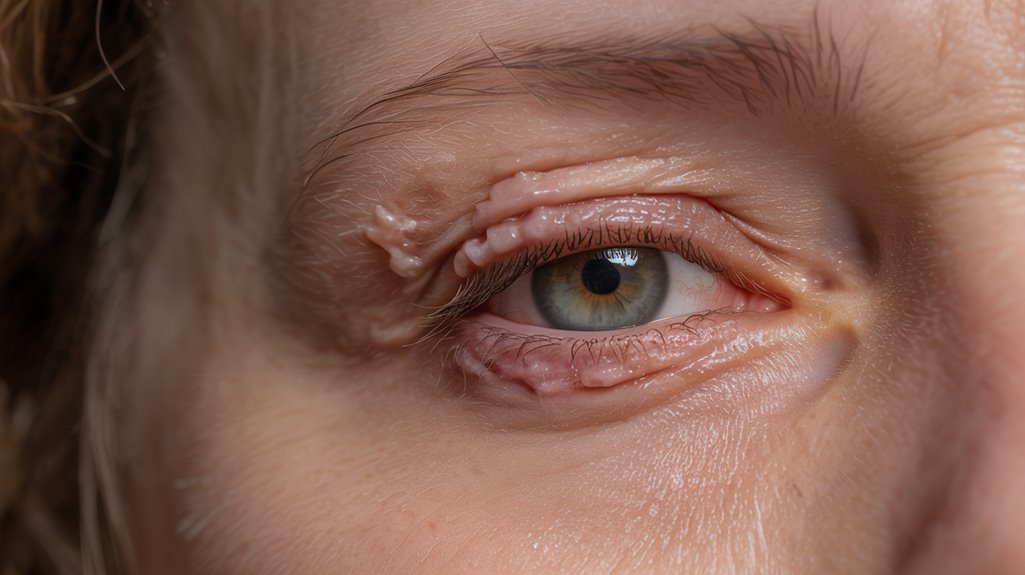
Redness and Swelling of the Eyelids
Redness and swelling of the eyelids often signify active inflammation in blepharitis, resulting from increased vascular permeability and localized immune responses at the lid margins. You’ll typically notice erythema and edema concentrated along the lash line, which may present bilaterally and fluctuate in intensity. These findings frequently correlate with exacerbations and can be confirmed on slit-lamp examination, revealing vascular engorgement and soft tissue thickening. Maintaining meticulous eyelid hygiene—such as regular cleansing with non-irritating solutions—plays a central role in reducing these inflammatory signs. When hygiene alone proves insufficient, treatment options may include topical antibiotics, corticosteroids, or immunomodulatory agents, based on clinical severity and underlying etiology. Early intervention mitigates the risk of chronic eyelid changes and secondary complications, emphasizing the importance of recognizing these specific symptoms. Approximately 30% of chronic cases of blepharitis involve Demodex mites, which can exacerbate inflammation and irritation, necessitating targeted treatment strategies.
Itching and Burning Sensations
Itching and Burning Sensations
Although often underestimated, itching and burning sensations along the eyelid margins are hallmark symptoms of blepharitis, reflecting underlying disruption of the lid’s barrier function and heightened local inflammatory mediators.
You may notice persistent pruritus and discomfort, driven by abnormal meibomian gland secretions and increased cytokine activity. This inflammatory response compromises ocular surface homeostasis, leading to sensory nerve irritation and subjective burning.
Itching relief often involves targeted lid hygiene, such as warm compresses and diluted baby shampoo, to reduce microbial load and debris. For burning treatments, clinicians may recommend artificial tears, topical corticosteroids, or immunomodulatory agents, depending on severity.
Prompt identification and intervention help prevent chronic symptoms and secondary complications. If you experience these sensations, consult an eye care provider for accurate diagnosis and management options. Regular eyelid hygiene with consistent routines can help manage symptoms effectively and reduce flare-ups.
Crusty or Flaky Eyelid Margins

Alongside itching and burning, you’ll often observe crusty or flaky debris accumulating along the eyelid margins in blepharitis. This debris typically consists of keratin, dried tears, and sebaceous secretions that collect at the base of your eyelashes.
The presence of these deposits can exacerbate inflammation and may contribute to bacterial overgrowth. Meticulous eyelid hygiene is critical—regularly cleansing the eyelid margins helps remove crusts, decreases microbial load, and reduces symptom severity.
Clinical studies indicate that warm compresses followed by gentle lid scrubs are effective first-line treatment options. In more persistent cases, clinicians may recommend topical or oral antibiotics to address underlying infection. Omega-3 fatty acids are known to support tear production and reduce inflammation, providing additional relief for individuals with blepharitis.
Watery or Dry Eyes
Many individuals with blepharitis notice significant changes in tear film stability, leading to symptoms of either excessive tearing (epiphora) or ocular dryness.
When you have blepharitis, inflammation of the eyelid margins disrupts the normal function of the meibomian glands, which are responsible for secreting the lipid layer of the tear film. This dysfunction can result in evaporative dry eyes, causing a gritty or foreign body sensation.
Paradoxically, the ocular surface may become so irritated that your lacrimal glands compensate by producing excess aqueous tears, leading to watery eyes.
Both watery eyes and dry eyes are hallmark manifestations of tear film instability associated with blepharitis. Recognizing these symptoms is essential for prompt diagnosis and targeted management of the underlying eyelid inflammation contributing to your discomfort. Additionally, blocked glands can exacerbate symptoms, leading to further complications and discomfort.
Sensitivity to Light
Photophobia, or sensitivity to light, frequently occurs in individuals with blepharitis due to chronic inflammation and disruption of the ocular surface.
When you experience blepharitis, the compromised tear film and inflamed eyelid margins can expose your corneal nerves, making your eyes more reactive to light stimuli. This heightened light sensitivity often presents as discomfort or pain when exposed to bright environments, such as sunlight or fluorescent lighting.
You may also notice increased eye strain during tasks that require visual concentration, especially in well-lit areas. Evidence indicates that persistent ocular surface inflammation plays a key role in photophobia associated with blepharitis. Regular use of Theralife products can improve symptoms, including light sensitivity, by promoting healing through natural ingredients.
Managing the underlying eyelid inflammation and maintaining ocular surface integrity are essential to reducing both eye strain and the intensity of light sensitivity in affected individuals.
Gritty or Foreign Body Sensation

You may notice a gritty sensation, often described as if sand is present in the eye, which is a hallmark of blepharitis. This persistent eye irritation results from chronic inflammation and debris along the eyelid margins. Clinical studies confirm that these symptoms frequently contribute to patient discomfort and decreased ocular surface health. It is important to understand that chronic dry eyes can create a cycle of inflammation that exacerbates blepharitis symptoms.
Sensation of Eye Sand
Patients with blepharitis frequently report a gritty or foreign body sensation, often described as the feeling of “eye sand.” This symptom arises from chronic inflammation of the eyelid margins, leading to disruption of the tear film and increased friction between the eyelid and ocular surface.
You may notice that this gritty sensation undermines your eye comfort, making daily activities challenging. The compromised tear film fails to adequately lubricate the ocular surface, exacerbating the sensation of particulate matter within the eye.
Clinically, this symptom signals the need to assess both the integrity of the tear film and the presence of debris along the lid margin. Implementing strict eyelid hygiene can help reduce debris and improve ocular surface health, thereby alleviating the “eye sand” sensation associated with blepharitis. Regular eyelid hygiene is crucial to minimize symptom recurrence and prevent further complications.
Persistent Eye Irritation
Alongside the sensation of “eye sand,” persistent eye irritation remains a hallmark symptom of blepharitis. You may experience a gritty or foreign body sensation, reflecting underlying chronic inflammation of the eyelid margins. This persistent discomfort is often exacerbated by environmental triggers such as wind or prolonged visual tasks. The table below summarizes clinical features, associated triggers, and patient-reported impacts:
| Clinical Feature | Trigger | Patient Impact |
|---|---|---|
| Grittiness | Wind exposure | Decreased focus |
| Foreign body feeling | Screen time | Frequent eye rubbing |
| Burning sensation | Air pollution | Sleep disruption |
| Redness | Contact lens use | Visual fatigue |
| Tearing | Low humidity | Reduced productivity |
Recognizing persistent eye irritation is essential for early diagnosis and targeted management of blepharitis-related chronic inflammation. Additionally, lifestyle adjustments like adequate sleep and hydration are crucial in supporting overall eye health and alleviating symptoms.
Eyelash Issues and Loss
Several eyelash abnormalities frequently accompany blepharitis, including misdirected growth (trichiasis), crusting, and partial or complete eyelash loss (madarosis).
You might notice disrupted eyelash growth, with lashes growing in the wrong direction, causing mechanical irritation to the ocular surface. Chronic inflammation often leads to weakened follicular support, resulting in lash fragility and shedding.
Proper eyelash care is essential to manage these complications and reduce the risk of further loss or infection. Clinically, these manifestations signify ongoing eyelid margin disease and may indicate the need for more intensive therapy. Misdirected lashes often require specialized treatments and careful management to prevent chronic ocular discomfort.
If left unaddressed, these changes can have significant functional and cosmetic impacts.
- Loss of eyelashes can undermine your confidence.
- Misdirected lashes may cause chronic discomfort.
- Crusting can make daily eyelash care challenging.
- Persistent eyelash issues might signal severe inflammation.
Blurred or Fluctuating Vision
You may experience blurred or fluctuating vision due to unstable tear film and ocular surface inflammation associated with blepharitis.
These visual disturbances can interfere with reading, driving, or computer work, impacting your daily function.
Effective symptom management often requires addressing underlying eyelid inflammation and optimizing tear film stability.
Causes of Blurred Vision
Although blepharitis primarily affects the eyelid margins, it can contribute to blurred or fluctuating vision due to the destabilization of the tear film and intermittent accumulation of debris on the ocular surface.
You may notice your vision becomes inconsistent, especially when inflammation is active. The principal causes of blurred vision in blepharitis stem from several pathophysiological mechanisms:
- Disrupted tear film stability, leading to optical irregularities and inconsistent refractive surfaces.
- Accumulation of inflammatory debris on the cornea, momentarily obstructing the visual axis.
- Meibomian gland dysfunction, resulting in insufficient lipid secretion and accelerated tear evaporation.
- Chronic ocular surface inflammation, which can directly impair corneal clarity.
Understanding these causes of blurred vision is essential for selecting effective treatment options, including lid hygiene, topical medications, and tear film stabilizers, to restore visual stability and ocular comfort.
Impact on Daily Tasks
When blepharitis leads to blurred or fluctuating vision, even routine visual tasks such as reading, driving, or screen use can become challenging.
You may notice that your ability to focus is inconsistent, particularly after prolonged periods of eye use or exposure to screens. This variability in visual acuity can cause daily discomfort and directly impact your productivity, especially when tasks require sustained attention or precision.
Clinical studies indicate that patients with blepharitis frequently report difficulty completing work-related assignments, experiencing eye fatigue, or needing to take frequent breaks.
These visual disturbances may also increase the risk of errors during detailed activities. Consequently, the persistent symptoms of blepharitis can greatly disrupt your daily functioning and diminish your overall quality of life.
Managing Visual Fluctuations
Since blepharitis commonly causes unstable tear film and inflammation along the eyelid margins, managing visual fluctuations requires a targeted approach that addresses both underlying inflammation and ocular surface irregularities.
You’ll notice that blurred or fluctuating vision often stems from tear film instability, leading to transient refractive changes.
Evidence-based management combines anti-inflammatory treatment options, such as topical antibiotics or corticosteroids, with meticulous lid hygiene.
Artificial tears and lubricating ointments help stabilize the tear film, while visual aids like prescription glasses may compensate for temporary changes in vision.
It’s crucial to tailor your regimen to symptom severity and persistence.
- Consult your ophthalmologist for personalized treatment options.
- Incorporate daily lid hygiene to minimize inflammation.
- Use preservative-free artificial tears for ocular surface support.
- Optimize visual aids to enhance clarity and comfort.
When to Seek Medical Attention
If you experience persistent eyelid irritation, worsening redness, vision changes, or develop painful swelling, these may indicate complications beyond typical blepharitis and require prompt medical evaluation. While most cases respond to standard treatment options, certain blepharitis triggers—such as bacterial infections or underlying dermatologic conditions—can escalate symptoms or cause secondary issues like corneal involvement. Timely assessment by an ophthalmologist guarantees early intervention and minimizes risk of vision-threatening sequelae. Pay attention to these warning signs:
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| Sudden vision changes | Corneal involvement | Seek urgent evaluation |
| Painful eyelid swelling | Abscess or severe infection | Consult specialist |
| Persistent redness | Chronic inflammation, allergy | Review treatment options |
Don’t delay when symptoms worsen or new ocular complaints emerge. Early intervention can optimize outcomes.
Frequently Asked Questions
Is Blepharitis Contagious to Other People?
You might wonder about Blepharitis transmission, but it’s generally not considered contagious between individuals.
Blepharitis commonly results from bacterial colonization, seborrheic dermatitis, or dysfunction of the meibomian glands, rather than direct person-to-person spread.
However, you should practice proper eyelid hygiene as a Blepharitis prevention measure.
Avoid sharing towels, cosmetics, or eye drops to minimize any theoretical risk of transmission of associated bacteria or irritants that could exacerbate the condition.
What Causes Blepharitis to Develop?
Blepharitis develops when you experience inflammation of the eyelid margins, typically due to bacterial colonization (often Staphylococcus species), seborrheic dermatitis, or dysfunction of the meibomian glands.
Other causes include Demodex mite infestation or allergic reactions.
Effective treatment targets the underlying etiology: improving eyelid hygiene, using topical or oral antibiotics, and sometimes anti-inflammatory agents.
You should consult an ophthalmologist for tailored treatment, since chronic cases may require ongoing management to control symptoms.
Can Blepharitis Affect Both Eyes at the Same Time?
You may experience blepharitis as a bilateral condition, meaning it often affects both eyes simultaneously.
Evidence shows that bilateral symptoms are common, presenting with persistent eye irritation, redness, and eyelid margin inflammation.
Clinically, the inflammatory process typically involves both upper and lower eyelids, suggesting a systemic or diffuse local cause rather than an isolated event.
Consequently, when you notice bilateral eye irritation, consider blepharitis as a potential etiology and seek ophthalmic evaluation.
Are Certain People More at Risk for Blepharitis?
Yes, you may be at higher risk for blepharitis if you have underlying dermatological conditions like rosacea or seborrheic dermatitis, a history of allergies, or poor eyelid hygiene.
Other risk factors include contact lens use and chronic dry eye.
To reduce your risk, follow prevention tips such as maintaining strict eyelid hygiene, managing skin disorders, and minimizing exposure to irritants.
Evidence shows these strategies can lower the incidence of blepharitis.
How Is Blepharitis Diagnosed by Doctors?
When your ocular comfort faces subtle challenges, doctors employ diagnostic methods rooted in evidence-based practice.
They’ll begin with a detailed eye examination, using slit-lamp biomicroscopy to scrutinize your eyelids, lashes, and tear film. Clinicians may gently express the meibomian glands to assess their function.
In some cases, they’ll collect samples for microbiological analysis. This systematic approach guarantees an accurate diagnosis and guides the best management for your ocular well-being.
Conclusion
When your eyelids show signs of blepharitis—such as redness, swelling, itchiness, or crusting—it’s crucial to address these symptoms promptly. Theralife offers a unique oral treatment for eye care, setting it apart as the sole provider of such a solution. This oral approach not only stabilizes the ocular surface but also enhances overall visual comfort, reducing the risk of chronic irritation and secondary complications. By choosing Theralife, you ensure that your eyes receive comprehensive care, maintaining their function and clarity for optimal vision.
References
- American Academy of Ophthalmology. Preferred Practice Pattern: Blepharitis. February 2024 revision. Available at: https://www.aao.org/education/preferred-practice-pattern/new-preferredpracticepatternguideline-4. Accessed August 18, 2025.
- Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012;5:CD005556.
- Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014 Oct;12(4):273-84. doi: 10.1016/j.jtos.2014.05.005. Epub 2014 Jul 22. PMID: 25284773.
- Rapuano Cj, Stout JT, Tsai LM, et al, eds. American Academy of Ophthalmology Basic Clinical Science Course: External Disease and Cornea. Vol. 8. San Francisco, CA: American Academy of Ophthalmology; 2025.
- Salmon JF. Kanski’s Clinical Ophthalmology (Tenth Edition). New York: Elsevier; 2024.
- Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocular Surface. 2009;7(Suppl 2):S1–14.
- Viso E, Rodríguez-Ares MT, Abelenda D, Oubiña B, Gude F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Invest Ophthalmol Vis Sci. 2012;53:2601-6.
- Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The International Workshop on Meibomian Gland Dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52:1994-2005.
- McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89:1173-80.
- McCulley JP, Dougherty JM. Blepharitis associated with acne rosacea and seborrheic dermatitis. Int Ophthalmol Clin. 1985;25(1):159–72.
- Baum J. Clinical manifestations of dry eye states. Trans Ophthalmol Soc U K. 1985;104(Pt 4):415-423.
- Bowman RW, Dougherty JM, McCulley JP. Chronic blepharitis and dry eyes. Int Ophthalmol Clin. 1987;27:27-35.
- Groden LR, Murphy B, Rodnite J, Genvert GI. Lid flora in blepharitis. Cornea. 1991;10(1):50–53.
- Huber-Spitzy, V., Baumgartner, I., Böbler-Sommeregger, K. et al. Blepharitis — a diagnostic and therapeutic challenge. Graefe’s Arch Clin Exp Ophthalmol 229, 224–227 (1991). https://doi.org/10.1007/BF0016787
- Helm KF, Menz J, Gibson LE, Dicken CH. A clinical and histopathologic study of granulomatous rosacea. J Am Acad Dermatol. 1991 Dec;25(6 Pt 1):1038-43. doi: 10.1016/0190-9622(91)70304-k. PMID: 1839796.
- Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, Powell F. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002 Apr;46(4):584-7. doi: 10.1067/mjd.2002.120625. PMID: 11907512.
- Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008 Nov;33(6):764-7. doi: 10.1111/j.1365-2230.2008.02892.x. Epub 2008 Jul 4. PMID: 18627384.
- Hu SW, Robinson M, Meehan SA, Cohen DE. Morbihan disease. Dermatol Online J. 2012 Dec 15;18(12):27. PMID: 23286817.
- Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): evidence of hidden immunologic contact urticaria and impaired lymphatic drainage. J Am Acad Dermatol. 2005 Apr;52(4):595-602. doi: 10.1016/j.jaad.2004.08.061. PMID: 15793508.
Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004 Dec;82(6):765-7. doi: 10.1111/j.1600-0420.2004.00335.x. PMID: 15606479.