Stop Crusty Eyes – Oral Therapy That Works.

- Crusty Sticky Build Up On Eyelids- Blepharitis
- Typical Problem with Dry Eyes
- Co-Exist with Clogged Oil Glands (MGD)
- Targets All 3 Root Causes Simultaneously
- Oral Capsules Restore from Inside Out. No more drops
- Prevents Recurrence
- 100% Money Back Guaranteed
Testimonial
“I had dry eyes before Lasik surgery in 2007. After Lasik, I was diagnosed with chronic dry eyes and blepharitis (crusty). My eyes were red, dry and painful. I tried many eye drops including prescription drop, antibiotic drops with no results. I started TheraLife Eye and can feel the difference in 2-3 weeks. I still cannot believe I have such total relief. I am so grateful for TheraLife.”
-C.L, Ohio
*Results may vary
Call and talk to a doctor if TheraLife is right for you- 1-877-917-1989 US/Canada
Why TheraLife Eye Protocol?
The TheraLife protocol treats dry eyes, blepharitis crusty eyes, MGD (clogged meibomian oil glands) at the same time for complete recovery. The high level of inflammation drives all three in a vicious cycle. To learn more, click here
What is in TheraLife Eye?
For a list of ingredients, Go to this web page and click “Ingredients”
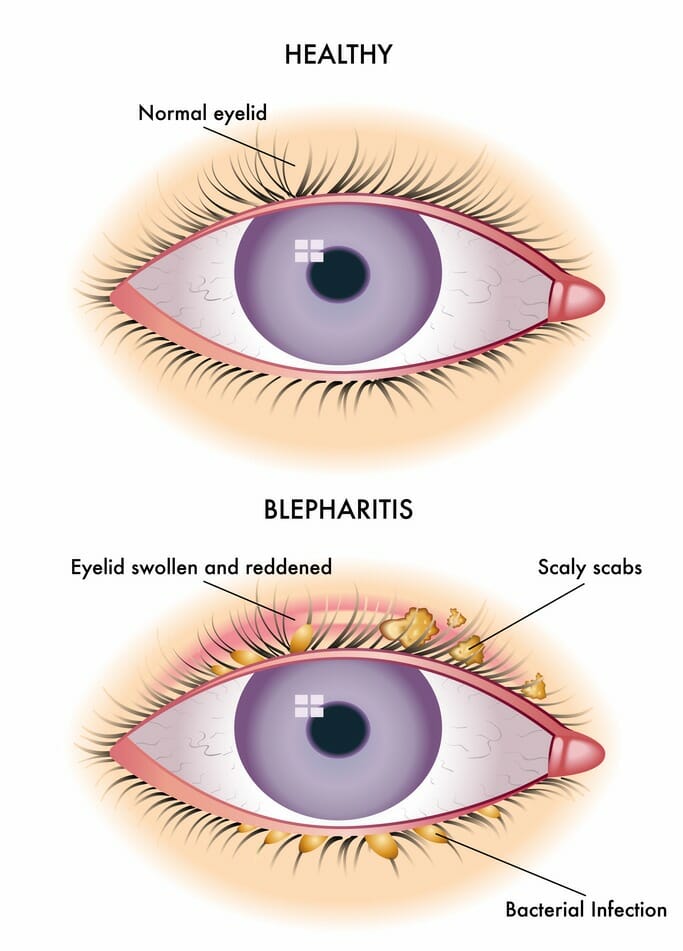
What Are Crusty Eyes
What are crusty eyes?
Crusty eyes here specifically refer to a condition called blepharitis. People who wake up with crusty eyes in the morning describe it as having their eyes glued shut.
There is typically eye gunk build-up on the eyelash line, a yellowish, sticky, crusty substance. This eye discharge condition can be temporary.
When do crusty eyes become chronic?
When eye discharge is persistent, you have a chronic condition requiring an eye doctor’s medical attention.
What is a sticky eye?
Sticky eyes are primarily due to allergies. It is not infectious, and antihistamines work well. Theralife Eye capsules also have strong anti-allergy components that allow you to relieve allergies naturally. More discussion is below.
Why Are Your crusty eyes Blepharitis So Chronic?
The root cause of chronic blepharitis is chronic dry eyes. The inflammation from dry eyes fuels the persistent inflammation of the eyelids.
Why crusty eyes (Blepharitis) cause clogged meibomian oil glands (MGD)
Blepharitis and dry eyes also cause meibomian gland dysfunction (MGD) – clogged oil glands that generally produce lubricants to thicken tears.
Why do dry eyes, crusty eyes, and blocked oil glands cause chronic conditions?
Dry eyes, blepharitis ( crusty eyes), and MGD all result in inflammation. Therefore we have a typical three-ring circus that each helps fuel the other in a vicious cycle.
And this is the reason why you have had blepharitis for so long, believing this will never stop.
How To Stop crusty eyes, Chronic Blepharitis- Abnormal Eye Discharge.
The only way to terminate this vicious cycle is to treat all three conditions simultaneously: dry eyes, blepharitis eye infection, and MGD.
To learn more – click here.
TheraLife Has The Perfect Solution To Stop Your Chronic Blepharitis.
Your all-natural solution
- Dry Eye Relief – TheraLife® Eye capsules– Restores and Revives the tear secretion glands intra-cellularly to relieve dry eyes all day long. With your very own tears.
- Meibomian Gland Dysfunction– Gel Warm Compresses– Regular warm compresses provide consistent, sustainable heat to melt and unclog the oil glands.
- Blepharitis– Use Avenova Eyelid Cleanser, which provides eyelid hygiene. Critical for blepharitis relief and complete recovery. Avenova builds up a biofilm layer to prevent bacteria from re-attaching to eyelids and re-infect. Cleaning eyelids with warm water or baby shampoo are not effective in stopping blepharitis recurrence.
- Lubrication – Use TheraLife Omega 3 Fish Oil to provide lubrication to thicken tears, relieve dry eyes, and reduce inflammation.
We highly recommend the discounted All-in-One Starter Kit that includes everything you need to achieve complete recovery from your crusty eye discharge.
What Causes Crusty Eyes?
Chronic dry eye is a major cause of chronic blepharitis. Other causes of blepharitis (crusty eye) include:
- conjunctivitis (pink eye), bacterial or viral eye infection, ocular herpes eye infection,
- allergies
- stye – also called a hordeolum.
What are crusty eyes a symptom of?
One common condition that may cause crusting around your eyes or eyelids is blepharitis or inflammation of the eyelids. Blepharitis can be a result of either bacterial eye infection or mites (Demodex). Blepharitis may cause your eyelids to stick together when you wake up.
What is the root cause of blepharitis?
The root cause of blepharitis is chronic dry eyes. Dry eyes result in inflammation which causes blepharitis and MGD.
How to treat crusty eyes -blepharitis?
Blepharitis may require medical attention. Proper eyelid hygiene can help limit this condition.
We highly recommend Avenova for lid hygiene.
What is the difference between crusty eyes and pink eye?
Blepharitis (crusty eye) is an irritation and inflammation of the eyelids. Conjunctivitis (pink eye) is an irritation and inflammation of the conjunctiva. The conjunctiva is the thin layer that covers the eye’s white and the eyelids’ inner surface.
Does blepharitis cause pink eyes?
Blepharitis crusty eyes can result in red eyes, not pink eyes. Pink eyes and crusty eyes due to blepharitis are different.
Can blepharitis turn into the pink eye?
Yes, blepharitis can lead to recurrent bouts of pink eye (conjunctivitis) and injury to the cornea.
Constant irritation from inflamed eyelids or misdirected eyelashes can cause a sore to develop on your cornea.
Does pink eye (Conjunctivitis) have abnormal eye discharge?
Pink eye- especially hyperacute bacterial conjunctivitis, is a severe eye infection that warrants immediate eye doctor and medical attention.
This bacterial conjunctivitis has an abrupt onset has a copious yellow or green eye gunk that comes back after being wiped away.
How Does Eye Gunk Form?
Where does eye gunk come from?
While we are awake, a tear film keeps our eyes moist and healthy. Blinking flushes out normal mucus produced by the conjunctiva, oil from the meibomian glands, and other debris from the front surface of the eye. It is normal and not from an eye infection.
Eye gunk forms when we do not blink during sleep. It collects in the corners of our eyes and along the eyelash line. A small amount of normal eye discharge is normal
When the discharge is yellow or green, you need to visit an eye doctor and get medical attention.
When Is Crusty Eye Discharge Abnormal
Having some eye discharge around your eyes, eyelids, and eyelashes is expected when you wake up. However, treatment will be necessary if you wake up with different-colored rheum, blurry vision, light sensitivity, or pain in your eyes. You could have an eye infection or other serious eye condition that requires a visit to your eye doctor.
Types of Eye Discharges
Depending on what is causing the eye discharge, additional symptoms may include:
- Blurred vision
- Burning sensation
- Itchy sensation
- Dry eyes
- Sore eyes
- Watery eyes from the blocked tear duct
- Red, crusty eyes
- Photophobia (light sensitivity) – a typical dry eye syndrome.
Complications from Abnormal Eye Discharge
- Blurry vision
- Spread of infection – especially bacterial or viral infections
- Crusty eyelids and chronic dry eyes can cause cornea damage if the cornea gets scratched.
- Loss of vision
- Dry, itchy eyes
- Inability to open eyelids in the morning
- Red, bloodshot eyes
Relief for Chronic Crusty Eyes
- Use wet warm compresses to soften the crust if your eyelids feel like they are glued shut to allow you to open your eyes.
- Stop using eye makeup, especially if you have chronic blepharitis.
- If you wear contact lenses, replace the cleaning and storage solutions daily. In severe cases, stop using contact lenses until you recover.
- Start a TheraLife® regimen today. The eyelid cleanser will remove excess oil and prevent bacteria and mites from attaching to your crusty eyelids. TheraLife® Eye Enhanced capsules will restore your tear secretion glands’ ability to produce normal tears for dry eye relief. START TODAY!
What are sticky eyes?
If you have allergies or a cold, you may have woken up with wet or crusted discharge in your eyes. This discharge can cause your eyes to become so wet or gummy that it may feel like your eyes are glued shut.
If you have sticky eyes, you have accumulated discharge — a collection of skin cells, debris, oil, and mucus — in the corner of your eyes. It’s often not a cause for alarm. Still, if it becomes consistent and excessive, sticky eyes can be a sign of an infection.
Sticky eye symptoms
The most common identifier of sticky eyes is a gummy discharge in the corner of your eye that may have spread across your eyelid. It’s important to take note of the color and consistency of this mucus. While occasional crusting is normal, abnormal colors accompanied with pain or excessive discharge should be discussed with your doctor, especially if they’re causing vision troubles. Some discharge colors or consistencies to look out for include:
- thick green or gray discharge
- thick, crusty discharge residue
- excessively watery discharge
- yellow discharge
Other symptoms you may experience with sticky eyes include:
- burning eyes
- dry eyes
- itchy eyes
- blurry vision
- pain
- light sensitivity
- red eyes
- flu symptoms
- inability to fully open your eyes
What causes your eyes to feel sticky?
Your eyes produce mucus throughout the day. It’s an essential part of normal tear production. This mucus — or discharge — helps to remove waste from your eyes and keeps your eyes lubricated. If your tear ducts become blocked, mucus can accumulate in the corner of your eye and spread, which occurs while you are sleeping.
The occasional crust from discharge is normal when waking up from a night’s rest. However, cases of abnormal discharge can have several contributing factors. Some conditions that may cause sticky eyes and excessive eye discharge include:
- poorly cleaned contact lenses
- pinkeye (conjunctivitis) — a viral or bacterial infection of the eye
- inflammation of the eyelids (blepharitis)
- styes
- eye ulcers
- dry eye syndrome
- tear duct infection (dacryocystitis)
- herpes virus in the eye
Treating sticky eyes
Treatment for sticky eye discharge depends on the underlying cause. Many home treatments can help with this condition. Before administering any treatment, make sure to wash your hands thoroughly to remove dirt, debris, and bacteria.
If your eyes are “glued shut” from dried discharge, take a warm washcloth and gently wipe your eyes. The warmth can loosen the crust from dried mucus, allowing your eyes to open. You can also use the warm washcloth as a compress to alleviate itching and irritation.
If your sticky eyes result from a bacterial infection, your doctor may prescribe antibiotic eye drops or ointments. If you’re experiencing sticky eyes from common allergies or a cold, over-the-counter (OTC), medication and antihistamines can help eliminate symptoms.
If you notice that you’re experiencing irregular symptoms after using facial products or makeup, stop use immediately and throw away any remaining products. These products may be irritating your eyes. If you’ve had an infection while using those makeup products, they may have become contaminated with bacteria.
It’s also essential to thoroughly clean and care for your contact lenses to prevent an infection.
Outlook
Sticky eyes and accompanying discharge are usually no cause for concern. They may even clear up on their own. However, your doctor may recommend medical treatment if you begin to experience worsening symptoms alongside heavy eye discharge.


Testimonial
"I am 6 months post LASIK. I was diagnosed with dry eyes and MGD. My eyes are red, inflamed with mucus. I can not begin to tell you how much Theralife has made a difference for my eyes! I'm still currently using 3-4 capsules twice daily, along with fish oil, warm compresses and daily eye hygiene with lid scrubs. My eyes have been feeling great! Thank you so much for caring. " Sincerely, Elise, , United States *Results may vary
Crusty Eyes: How TheraLife® Eye Can Help
If you are visiting this page because you have crusty eyes, you may have Blepharitis or Meibomian Gland Dysfunction – some of the most difficult dry eye conditions to treat.
You may have already tried eye drops, antibiotics, and steroids to no avail.
TheraLife® Eye is doctor-recommended and clinically proven to work for 80% of first time users.
Get Help Today – Call Toll Free 1-877-917-1989
References
1. Bowling JJ. Clinical Ophthalmology: A Systemic Approach. 7th ed. New York: Elsevier Saunders; 2011. pp. 34–39.
2. Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocular Surface. 2009;7(Suppl 2):1–14.
3. Nelson JD, Shimazaki J, Benitez-del Castillo JM, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthal Vis Sci. 2001;52(4):1930–1937.
4. Nemet AY, Vinker S, Kaiserman I. Associated morbidity of blepharitis. Ophthalmology. 2011;118(6):1060–1068.
5. McCulley JP, Dougherty JM. Blepharitis associated with acne rosacea and seborrheic dermatitis. Int Ophthalmol Clin. 1985;25(1):159–172.
6. Groden LR, Murphy B, Rodnite J, Genvert GI. Lid flora in blepharitis. Cornea. 1991;10(1):50–53.
7. Huber-Spitzy V, Baumgartner I, Bohler-Sommeregger K, Grabner G. Blepharitis – a diagnostic and therapeutic challenge: report on 407 consecutive cases. Graefes Arch Clin Exp Ophthalmol. 1991;229(3):244–247.
8. Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010;25(3):79–83.
9. McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89:1173–1180.
10. American Academy of Ophthalmology Preferred Practice Pattern: Blepharitis. Oct, 2012. [Accessed November 10, 2014]. revision. Available from:
11. Din N, Patel NN. Blepharitis – a review of diagnosis and management. Int J Ophthalmol Prac. 2012;3(4):150–155.
12. Duncan K, Jeng BH. Medical management of blepharitis. Cur Opin Ophthalmol. 2015;26(4):289–294.
13. Scheinfeld N, Berk T. A review of the diagnosis and treatment of rosacea. Postgrad Med. 2010;122(1):139–143.
14. Probst LE. Bacterial eyelid infections. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. Philadelphia, PA: Elsevier Mosby; 2005. pp. 495–500.
15. McCulley JP. Blepharoconjunctivitis. Int Ophthalmol Clin. 1984;24(2):65–77.
16. Ficker L, Ramakrishnan M, Seal D, Wright P. Role of cell-mediated immunity to staphylococci in blepharitis. Am J Ophthalmol. 1991;111(4):473–479.
17. Jackson WB. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol. 2008;43(2):170–179.
18. Raskin EM, Speaker MG, Laibson PR. Blepharitis. Infect Dis Clin North Am. 1992;6(4):777–787.